Ever been handed a bright orange Omnicef capsule and wondered why this antibiotic pops up so often at the pharmacy? It’s not just you. In the UK and beyond, Omnicef—otherwise known as cefdinir—has quietly become one of the go-to antibiotics for fighting certain bacterial infections. Yet, tons of people still aren’t quite sure what makes it tick (or whether it’s the right choice for their chest infection or their kid’s earache). There’s more to this little capsule than meets the eye. After all, knowing the what, how, and why of Omnicef can mean the difference between a smooth recovery and weeks of unnecessary worry.
What Is Omnicef and How Does It Work?
First things first: Omnicef is the brand name for cefdinir. This isn’t your classic penicillin. It’s in the cephalosporin family—a group of antibiotics that’s often used when someone can’t take penicillin due to an allergy or when typical antibiotics aren’t hitting the mark. What’s unique about cefdinir is its broad-spectrum nature. It can handle a range of bacteria, especially in the respiratory tract. Think sinus infections, strep throat, tonsillitis, mild pneumonia, or those infamous childhood ear infections. Doctors in both the US and UK like it for tricky cases where other meds haven’t done the trick (or when they want to avoid amoxicillin for the fifth time in a year).
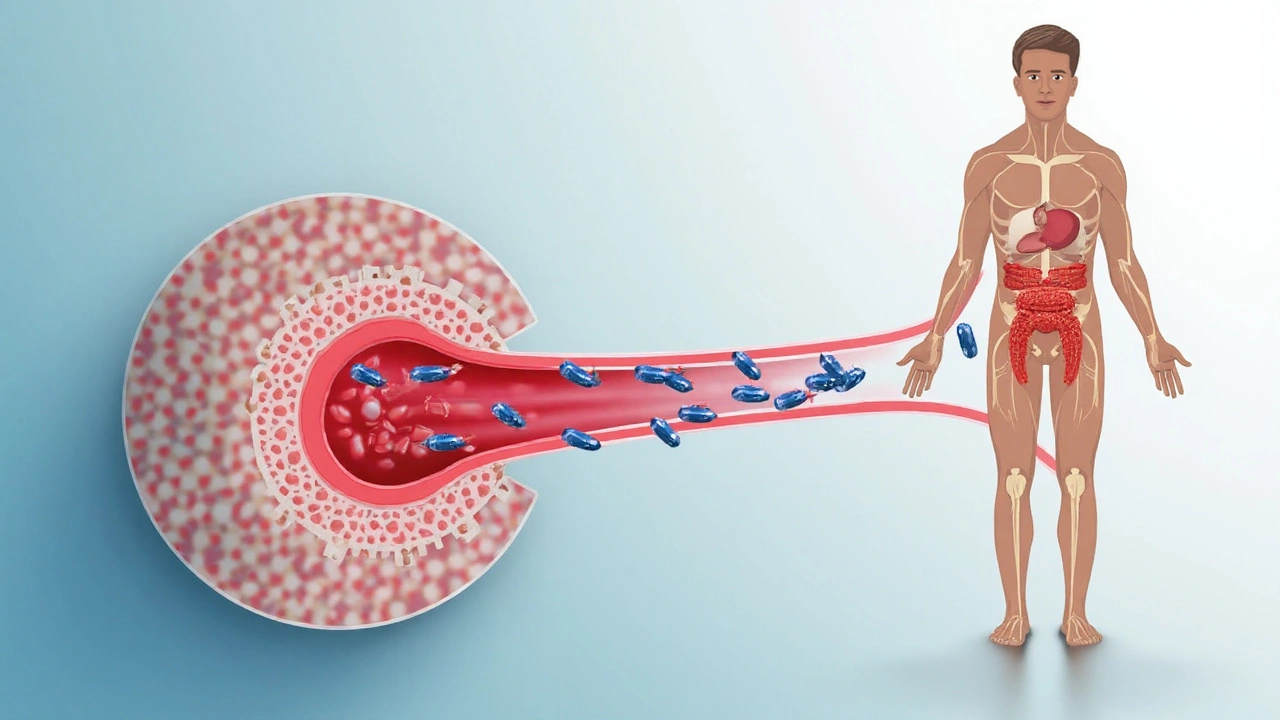
How does it actually work? Simply put, Omnicef slips in and messes with bacteria so they can’t build strong cell walls. Without sturdy walls, the bacteria can’t survive. What’s nice is that Omnicef usually doesn’t mess with “good” gut bacteria to the same extent as older, more aggressive antibiotics. Less disruption, fewer gut issues—at least most of the time.
Fun fact: Cefdinir first showed up on pharmacy shelves in 1991, and was approved for use in the US in 1997. Since launch, prescriptions have boomed—especially in paediatrics—thanks to a gentler profile compared to some tougher antibiotics. But, and here’s the catch, it only works against bacteria, not viruses. So using it on viral colds or the flu? That’ll just feed antibiotic resistance, making it less useful for everyone when we truly need it.
Here’s a quick look at some of the infections Omnicef is most commonly prescribed for:
| Infection | How Often Omnicef Used |
|---|---|
| Ear infections (otitis media) | Frequently, especially in children |
| Sinusitis | Moderate to frequent |
| Bacterial bronchitis | Common choice |
| Tonsillitis/pharyngitis (strep throat) | Common, especially with allergies to penicillin |
| Pneumonia (mild cases) | Less common, but still used |
Who Should Take Omnicef (and Who Really Shouldn’t)?
Omnicef isn’t a ‘one size fits all’ sort of antibiotic. Your GP or nurse practitioner will look at your medical history, allergies, and the infection’s likely cause. Omnicef is usually a winner for otherwise healthy folks—kids included—facing standard respiratory infections. It gets bonus points for kids since it comes in a sweet, liquid suspension (no more fighting over swallowing giant pills!).
But there are groups who need to steer clear—or at least, tread carefully. Anyone with a known allergy to cephalosporins, or even severe reactions to penicillin, should flag it straight away. Some folks with chronic kidney disease or reduced kidney function should avoid Omnicef or have their dose tweaked, as it can build up in the body and cause problems if the kidneys can’t flush it out properly.
Pregnant or breastfeeding? The safety data is actually pretty comforting: animal studies haven’t shown harm to developing babies, and doctors have safely prescribed it to pregnant women when the benefits outweigh the risks. But it’s not a medicine you should start without a proper conversation with your GP.
Here’s a handy checklist to figure out whether Omnicef might be the right fit (though always double-check with your prescriber):
- Have an infection confirmed (preferably with a swab/culture, especially if chronic or severe).
- No known allergy to cephalosporins or severe amoxicillin allergy.
- Kidney function is normal, or the dose is adjusted for impairment.
- Not currently taking iron supplements or antacids (more on this in a tick).
- Over age 6 months (it’s not for babies under 6 months).
If any of these trips you up, don’t panic—there are usually alternatives. But, don’t try to decide on your own whether to keep taking a prescribed course or to stop. That’s where resistance builds, and you really don’t want that on your conscience.
Taking Omnicef: How to Get the Best Results
Just because you’ve got a magic capsule in your hand doesn’t mean the bugs are gone overnight. First tip: finish the course, even if you’re feeling better, unless your doctor tells you otherwise. Most courses last five to ten days. Stopping halfway because you feel fine is a surefire way to invite those bacteria back for a second, tougher round.
Food isn’t a big deal with Omnicef—it can be taken with or without meals. That being said, if you’ve got a sensitive stomach, taking it with a snack usually helps. Here’s something most people miss: don’t wash it down with antacids, iron tablets, or calcium supplements. These can bind the medicine and keep it from soaking in properly. Best bet is to separate Omnicef from those by at least two hours.
Missed a dose? The old “double up” doesn’t work well here. If you miss one and it’s only been a couple of hours, take it as soon as you remember. If you’re close to your next scheduled dose, just skip and carry on. Don’t try to catch up by taking extra, or you’ll risk a nasty stomach ache and possibly other side effects.
Store the liquid version in the fridge if you’re using it for a child, but don’t freeze it. Always shake it before dosing. Use the proper measuring spoon or syringe, not your average kitchen teaspoon—they vary too much, and accurate dosing is key for antibiotics. Toss any unused liquid after ten days—it loses potency even if it looks the same.
Keeping a simple log on your phone or a sticky note can help you keep track of doses if you’re prone to forgetting. And as anyone who’s given medicine to a toddler knows… bribery with stickers or chocolate buttons works wonders.
Possible Side Effects, Red Flags, and What To Do About Them
No one loves side effects, but with Omnicef, most people get off lightly. The most frequent issues are mild: tummy ache, loose stools, a bit of nausea. These usually pass on their own or can be helped by sticking to bland foods and staying hydrated. Yeast infections (like thrush in women) can crop up, especially after several days, but a quick trip to the chemist usually sorts that out.
Serious reactions are rare but not unheard of. Watch for signs of an allergy—rash, swelling of lips/tongue, difficulty breathing—or severe, watery diarrhoea that doesn’t stop. Stopping the medicine and ringing your GP or 111 straight away is the right call. Omnicef is known for giving some kids weird, reddish poop, especially if they’re on iron-fortified formula or vitamins. It looks alarming, but it’s harmless.
Here’s a round-up of known side effects and how often they show up, based on clinical trial data and post-marketing surveillance:
| Side Effect | Frequency |
|---|---|
| Nausea | ~3-5% |
| Headache | ~2-3% |
| Loose stools/diarrhoea | ~5-8% |
| Vaginal yeast infection | ~1-2% (usually women) |
| Serious allergic reaction (anaphylaxis) | Very rare (~0.01%) |
A little practical tip: probiotics (yogurts with live cultures, or over-the-counter capsules) might help keep the gut on an even keel, especially if you’ve had gut trouble with antibiotics in the past. Just make sure to time them at least two hours apart from Omnicef so they’re not wiped out by your own medicine!
Developing any unusual symptoms while taking Omnicef—even if they seem unrelated—should prompt a quick call to your prescriber. And don’t forget to mention it during medication reviews if you’ve ever had weird reactions to *any* antibiotics.

Brent Herr
August 13, 2025 AT 19:52Nice overview but a quick reality check: people keep popping antibiotics like candy and then acting surprised when they stop working.
Using Omnicef responsibly is the bare minimum. If your GP gives it to you for a likely bacterial infection, fine — take it properly. If you just want it because your throat is sore and it's probably viral, stop asking for antibiotics. You're not smarter than the microbiologist who warns about resistance.
Also: finish the course unless a clinician tells you otherwise. Half-measures are how resistant strains spread. End of rant.
Vic Harry
August 15, 2025 AT 21:52Don't take antibiotics for a cold.
Suman Wagle
August 17, 2025 AT 23:52Good write-up and a reminder that medicine sits between two uncomfortable truths: the urge to act quickly and the need to act correctly.
We want immediate fixes, but bacteria don't care about our impatience. They only care about survival, and when we feed them half-finished courses or use antibiotics for viruses, we're training them, unintentionally, to persist.
Also, it's a small comfort to parents that Omnicef tastes okay — the real victory is not giving it when it's unnecessary. If your child gets better on day two, still follow the plan the clinician gave. It's the long view that matters, not the quick reassurance.
And for those worried about side effects: watch the stools if someone's on iron, it's weird but usually harmless. If symptoms turn nasty, that's when the conversation with a prescriber needs to happen.
Bradley Fenton
August 20, 2025 AT 01:52Short tip: separate Omnicef and iron/antacids by two hours.
Liquid should be refrigerated and tossed after 10 days.
Wayne Corlis
August 22, 2025 AT 03:52This post hits a lot of the practical points, but let's unpack a few things in more detail because people tend to skim and then do the wrong thing anyway.
First, the mechanism: cephalosporins like cefdinir inhibit cell wall synthesis by binding to penicillin‑binding proteins. That is a dull way of saying they punch holes in the bacteria’s defensive armour, which leads to bacterial death if the organism is susceptible. Sounds technical, but the implication is simple — if the bug is resistant or not the right species, the drug does nothing, and you’ve only exposed your microbiome to unnecessary pressure.
Second, the whole allergy angle is messier than most people assume. A lot of patients claim penicillin allergy but aren't truly allergic; many had rashes as kids, or vague reactions that weren't immune mediated. That history matters because cephalosporins are often avoided unnecessarily, and avoiding them can lead to use of broader drugs with worse side effect profiles and greater selection pressure for resistance.
Third, the dosing nuance: renal function matters. If kidneys are impaired, cefdinir can accumulate — not everyone realizes that dosage adjustment is more than an academic note. Pharmacokinetics change with age and comorbidities, so what’s written on the leaflet can be a starting point but not gospel for everyone.
Fourth, the iron interaction is a nerdy but important point. The red stool phenomenon with iron plus cefdinir in kids looks scary to parents — and yes, it’s benign — but it's also illustrative of how drug–food interactions can alter appearance and cause unnecessary ER visits. Educating caregivers about this could save a lot of anxiety.
Fifth, about probiotics: they can help, but timing is key. Taken too close to the antibiotic and they might not colonize effectively. Space them out and aim for products with documented strains if you want a better chance of benefit.
Sixth, public health: the more we overuse these molecules, the fewer will work when we need them. That’s not hyperbole; it's the calculus staring clinicians in the face every day.
Finally, it’s worth remembering that guidelines evolve. What was standard five years ago might be tweaked today based on resistance patterns. If you’re prescribed Omnicef, trust your clinician but ask why it was chosen and what alternatives exist. Knowledge is the best way to ensure antibiotics are used responsibly.
Kartikeya Prasad
August 24, 2025 AT 05:52Very thorough post and the prior comment nails the kidney/dosing bit.
Quick grammar-and-safety friendly reminder: always ask the prescriber about interactions, and don't be shy about getting the name of the specific bacteria if a culture was done — it helps you look up susceptibility later if needed 🙂
Wayne Corlis
August 26, 2025 AT 07:52Totally agree — knowing the organism and the susceptibility pattern changes the conversation from guesswork to evidence. When cultures are negative or not done, empiric therapy is reasonable, but we should always reassess once lab results are in.
Also, a small practical thing: if your kid gets a rash after starting Omnicef, don't leap to conclusions. Some rashes are benign and non‑allergic; others need urgent attention. Context matters: timing, progression, systemic features. Ask the clinician whether to stop the drug, not the internet.
HARI PRASATH PRASATH
August 28, 2025 AT 09:52why ppl keep taking antibiotics without tests is beyhond me lol
if doc says dont give em, dont give em. simple
Andrew Miller
August 30, 2025 AT 11:52Yeah, but try telling that to someone convinced their sore throat is a bacterial plot.
June Wx
September 1, 2025 AT 13:52Love that the article mentioned the orange capsule — small details matter. Makes the info feel real.
Also, a PSA: if you're on Omnicef and notice vaginal yeast issues, don't freak — antifungal treatments at the chemist often sort it out quick.
Caitlin Downing
September 3, 2025 AT 15:52Good point — and if anyone's unsure about whether symptoms are yeast-related or antibiotic-related, a quick photo for the pharmacist or a short call to the clinic can clarify. No shame in asking.
One tiny nit: the article said "toss liquid after ten days" which is spot-on — but remind caregivers to note the prep date right away. It's easy to lose track and assume it's fine when potency has dropped.
Bradley Fenton
September 5, 2025 AT 17:52Another quick practical: use an oral syringe for kids. Kitchen spoons lie — badly. Accuracy matters for dose and to avoid underdosing which breeds resistance.
Suman Wagle
September 7, 2025 AT 19:52Right — and that small act of measuring properly is almost philosophical if you think about it. The tiny precise dose you give today can have ripple effects in community resistance years down the line.
Better to be pedantic about measurement than casual about consequences.
Brent Herr
September 9, 2025 AT 21:52Also, cut the nonsense about hoarding antibiotics or using leftovers from last illness. That’s reckless. If you can't see a GP, ask a pharmacist — many can advise whether you need referral or tests.
And if you do pick up Omnicef, read the leaflet. Yes, it's boring, but it's also the difference between a smooth recovery and a mess that drags on. You owe that small effort to everyone around you.
Vic Harry
September 11, 2025 AT 23:52Simple: listen to professionals, finish the course, don't self-prescribe.