Cyclosporine Drug Interaction Checker
Check Medication Safety
When you take cyclosporine, you're not just managing your immune system-you're navigating a minefield of hidden drug interactions. This powerful immunosuppressant, used after organ transplants and for autoimmune diseases like psoriasis and rheumatoid arthritis, doesn't just sit quietly in your body. It actively interferes with how your liver and gut process dozens of other medications. The culprit? Its strong inhibition of the CYP3A4 enzyme, which handles about 60% of all prescription drugs you might be taking. This isn't theoretical. People get hospitalized because of it. And many don’t even know why.
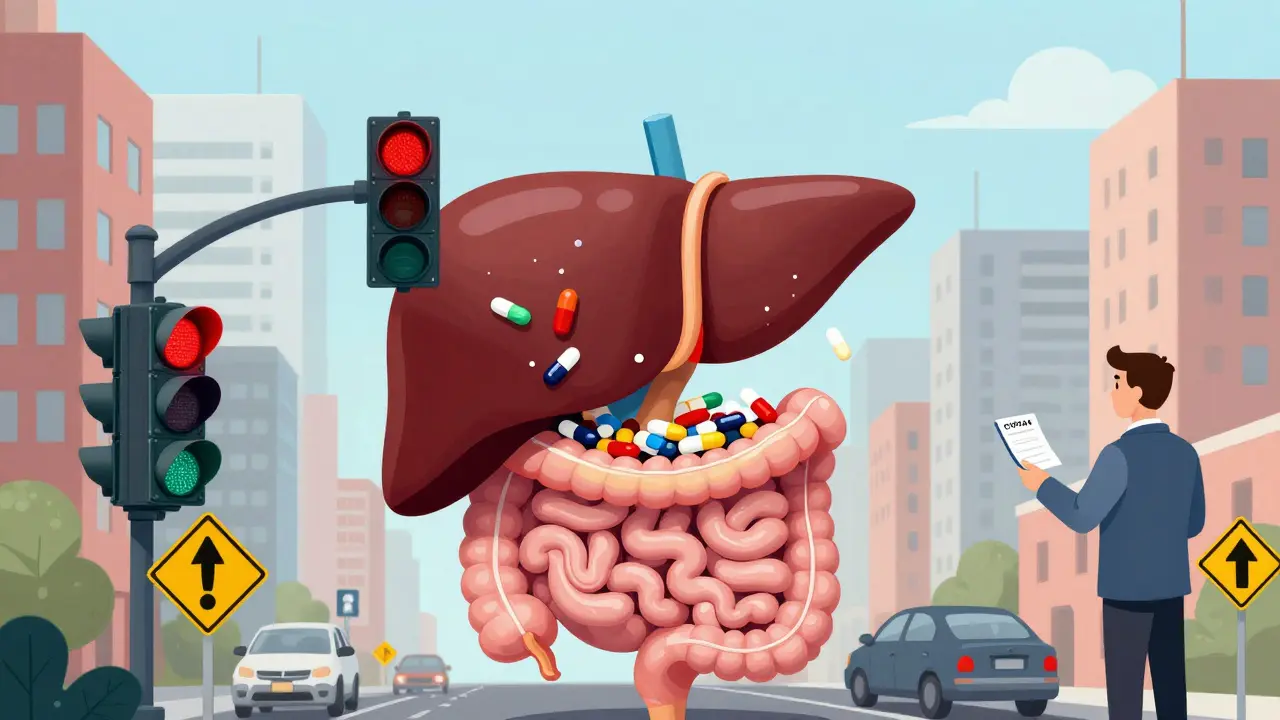
What CYP3A4 Does-and Why It Matters
CYP3A4 is the workhorse of your body’s drug-processing system. Found mostly in your liver and intestines, this enzyme breaks down medications so they can be cleared from your body. Without it, drugs like statins, blood pressure pills, and even some antibiotics would build up to dangerous levels. But when cyclosporine steps in, it blocks CYP3A4 from doing its job. The result? Other drugs stick around longer than they should, and their concentrations can spike-sometimes doubling or tripling. That’s not a minor issue. It’s the difference between a safe dose and a toxic one.
Think of it like traffic control. CYP3A4 is the traffic light that lets drugs pass through your system. Cyclosporine doesn’t just slow the light-it turns it red permanently for certain drugs. And unlike some inhibitors that wear off quickly, cyclosporine’s effect lasts as long as you’re taking it. Even small changes in your other meds can trigger serious side effects.
How Cyclosporine Inhibits CYP3A4-It’s Not Just One Way
Many people assume drug interactions are simple: one drug blocks another. But cyclosporine’s action is more complex. It doesn’t just compete for space on the enzyme like a typical inhibitor. Research shows it acts as a mixed inhibitor, meaning it binds to CYP3A4 in multiple ways-sometimes blocking the active site, other times changing the enzyme’s shape so it can’t function properly. This makes its effects harder to predict.
Even more concerning is evidence that cyclosporine causes mechanism-based inhibition. This means the drug gets turned by CYP3A4 into a reactive compound that permanently damages the enzyme. Your body has to make new enzyme molecules to recover, which can take days. So if you start a new medication while on cyclosporine, the interaction doesn’t just happen right away-it builds over time. That’s why some patients feel fine at first, then suddenly develop kidney damage or muscle pain a week later.
Drugs That Become Dangerous with Cyclosporine
Here’s what you need to watch out for. These are not rare cases. These are common medications that interact with cyclosporine in predictable, documented ways:
- Statins (simvastatin, lovastatin, atorvastatin): These cholesterol drugs are metabolized almost entirely by CYP3A4. When combined with cyclosporine, their levels can rise 10-fold. That raises the risk of rhabdomyolysis-a life-threatening muscle breakdown. Even low-dose statins can be dangerous.
- Calcium channel blockers (diltiazem, verapamil, nifedipine): Used for high blood pressure and heart rhythm issues, these can increase cyclosporine levels by 30-50%. The reverse is also true: cyclosporine makes these drugs more potent, leading to low blood pressure or heart rhythm problems.
- Antifungals (ketoconazole, itraconazole): These are strong CYP3A4 inhibitors themselves. Combine them with cyclosporine, and you’re stacking two inhibitors. This can push cyclosporine levels into toxic range, causing kidney failure.
- Sirolimus and everolimus: These immunosuppressants are often used after transplants. Cyclosporine increases their blood levels by over 2-fold. Doctors usually cut sirolimus doses by 70% when used with cyclosporine.
- Some antidepressants and antipsychotics (sertraline, quetiapine): These can accumulate and cause dizziness, confusion, or seizures.
And don’t forget about grapefruit juice. It’s a well-known CYP3A4 inhibitor. One glass with your cyclosporine can raise its concentration enough to require an emergency dose reduction.
Cyclosporine vs. Tacrolimus: A Key Difference
Many patients are switched from cyclosporine to tacrolimus because it’s considered more effective. But here’s the twist: tacrolimus doesn’t inhibit CYP3A4. It’s a substrate-meaning it gets broken down by the enzyme, not blocks it. So if you’re on tacrolimus, your risk comes from other drugs that inhibit CYP3A4 (like clarithromycin or fluconazole). But with cyclosporine, you’re the one doing the blocking. That means you’re not just at risk from other drugs-you’re making other drugs more dangerous.
This is why transplant teams track both drugs differently. If a patient on tacrolimus starts an antibiotic, the team lowers the tacrolimus dose. If a patient on cyclosporine starts the same antibiotic, they might need to lower the antibiotic dose instead. The logic flips.
Why Genetic Differences Make It Worse
Not everyone metabolizes cyclosporine the same way. Some people have genetic variants of CYP3A4 that make the enzyme less active. Others have extra copies that work faster. Studies show certain variants can reduce CYP3A4 activity by up to 40%. That means two people on the same cyclosporine dose can have wildly different blood levels.
And here’s the catch: if you’re a slow metabolizer, cyclosporine stays in your system longer. That means more time for it to block CYP3A4 and affect other drugs. A 2023 study from Wenzhou Medical University found that patients with these genetic differences needed dose adjustments 3 times more often than others. Yet, most clinics still don’t test for this. If you’ve been on cyclosporine for more than a year and still have unexplained side effects, ask about pharmacogenetic testing.
Real-World Consequences: What Happens When Things Go Wrong
In 2021, a multicenter study of 1,245 kidney transplant patients found that over one-third had at least one serious drug interaction involving cyclosporine. Nearly 1 in 12 ended up in the hospital. Common outcomes? Kidney damage, muscle breakdown, abnormal heart rhythms, and high blood pressure.
One case involved a 58-year-old man on cyclosporine after a heart transplant. He started taking a common antifungal for athlete’s foot. Within 72 hours, his cyclosporine level spiked to 800 ng/mL-more than double the safe limit. He developed acute kidney injury and needed dialysis. He survived, but his recovery took months.
On the flip side, stopping a CYP3A4 inhibitor can be just as dangerous. If you’re on cyclosporine and a doctor takes you off a strong inhibitor like clarithromycin, your CYP3A4 enzyme starts working again. Cyclosporine gets cleared faster. If you don’t adjust your dose, your levels can crash. That’s when rejection happens. One patient lost a liver transplant because his doctor didn’t realize the antibiotic he’d stopped was the reason his cyclosporine level had dropped.
How to Stay Safe: What You Need to Do
There’s no magic solution. But you can drastically reduce your risk with these steps:
- Keep a complete list of every medication, supplement, and herb you take-including over-the-counter drugs and natural remedies. Share it with every doctor and pharmacist.
- Ask before starting anything new. Even a simple painkiller like ibuprofen can affect kidney function when combined with cyclosporine. Don’t assume it’s safe.
- Get your cyclosporine levels checked regularly. Trough levels should be monitored weekly when starting or changing other meds, then monthly once stable. Target levels vary by transplant type but usually fall between 100-400 ng/mL.
- Know the warning signs: Unexplained muscle pain or weakness, dark urine, swelling in your legs, sudden fatigue, or confusion could mean toxicity.
- Use a drug interaction checker-but don’t rely on it alone. Tools like the University of Washington’s Drug Interaction Checker are reliable, but they need internet access. Ask your pharmacist for a printed list of dangerous combos.
The Future: Personalized Dosing and Real-Time Monitoring
Transplant centers are starting to use algorithms that combine your genetics, age, weight, kidney function, and current meds to predict your ideal cyclosporine dose. Early models are 85-90% accurate. That’s a big leap from trial-and-error.
Point-of-care blood tests are also on the horizon. Prototype devices can measure cyclosporine levels from a finger prick in under 10 minutes, with accuracy matching lab tests. These are in phase 3 trials and could be in clinics by 2027. Imagine knowing your level before you leave the doctor’s office.
For now, the best tool is awareness. Cyclosporine saved millions of lives. But it demands respect. Treat every new medication like a potential landmine. Your life depends on it.
Can I take ibuprofen with cyclosporine?
Ibuprofen isn’t a CYP3A4 inhibitor, but it can still be risky with cyclosporine. Both drugs stress the kidneys. Taking them together increases the chance of kidney damage, especially if you’re dehydrated or already have reduced kidney function. Most doctors avoid combining them. If you need pain relief, acetaminophen (paracetamol) is usually safer-but always check with your transplant team first.
Does grapefruit juice really affect cyclosporine?
Yes, and it’s not a myth. Grapefruit juice contains compounds that block CYP3A4 in your gut, which is where cyclosporine is absorbed. Just one glass can raise cyclosporine levels by 30-50%. The effect lasts over 24 hours. Even small amounts matter. If you’re on cyclosporine, avoid grapefruit, Seville oranges, pomelos, and their juices entirely.
Why do some people on cyclosporine get high blood pressure while others don’t?
Cyclosporine itself can raise blood pressure by narrowing blood vessels and affecting kidney function. But if you’re also taking a CYP3A4 substrate like diltiazem or verapamil, the interaction can make this worse. Some people are genetically more sensitive to cyclosporine’s vasoconstrictive effects. Others may have underlying kidney disease or are on higher doses. Monitoring blood pressure daily and adjusting meds based on levels is key.
Can I switch from cyclosporine to tacrolimus to avoid interactions?
Switching is common, but it’s not a simple fix. Tacrolimus is less likely to cause drug interactions because it doesn’t inhibit CYP3A4. But it’s still a CYP3A4 substrate, so it’s vulnerable to other inhibitors. Also, tacrolimus has its own side effects-higher risk of diabetes and tremors. The decision to switch depends on your transplant type, kidney function, and how well you tolerate cyclosporine. Never switch without close supervision from your transplant team.
How often should I get my cyclosporine levels checked?
When you start cyclosporine or change any other medication, check levels every 2-3 days for the first week, then weekly for the next month. Once stable, monthly checks are usually enough. But if you get sick, start a new antibiotic, or change your diet (like eating more grapefruit), get tested immediately. Levels can shift fast.
Are there any supplements I should avoid with cyclosporine?
Yes. St. John’s wort reduces cyclosporine levels by inducing CYP3A4, which can lead to transplant rejection. Garlic, echinacea, and green tea extract can also interfere with metabolism or increase bleeding risk. Even fish oil in high doses may affect kidney function. Always tell your pharmacist about supplements-many don’t appear on standard interaction checkers.
Jim Johnson
February 11, 2026 AT 19:27Man, this post is a lifesaver. I’ve been on cyclosporine for 5 years post-kidney transplant, and no one ever told me about the grapefruit juice thing until I got hospitalized. Now I drink water like it’s my job. If you’re on this med, treat every new pill like a stranger at a party-don’t let them in without checking first.