Getting a vaccine while on blood thinners doesn’t mean you have to skip it. But if you’ve ever come home with a huge bruise after a shot, you know why people worry. The good news? You can get vaccinated safely-if you and your provider follow the right steps. It’s not about avoiding the shot. It’s about getting it right.
Why Blood Thinners Make Vaccines Riskier
Blood thinners like warfarin, rivaroxaban, and apixaban stop clots from forming. That’s lifesaving for people with atrial fibrillation, deep vein clots, or artificial heart valves. But it also means your body doesn’t seal up small breaks as quickly. When a needle goes into your muscle for a vaccine, it creates a tiny wound. Normally, that heals fast. With blood thinners, it can bleed a little longer under the skin. That’s what causes bruising-or worse, a hematoma, a swollen, painful lump filled with blood.It’s not common. CDC data shows only 1.2% of people on blood thinners report serious complications after vaccines. But for those who do, it’s painful, slow to heal, and can lead to unnecessary ER visits. The key isn’t avoiding vaccines. It’s controlling how the shot is given.
What Vaccines Are Safe?
All routine vaccines are safe for people on blood thinners. That includes:- Influenza (flu shot)
- COVID-19 boosters (Pfizer, Moderna)
- Pneumococcal (Prevnar, Pneumovax)
- Tdap (tetanus, diphtheria, pertussis)
- Shingles (Shingrix)
There’s no vaccine you should skip because you’re on anticoagulants. In fact, you’re at higher risk for complications from these diseases. Flu can lead to pneumonia. Shingles can cause nerve damage. COVID-19 is more dangerous if you have heart or lung conditions-which many people on blood thinners already have.
Early in the pandemic, some doctors held off on shots. That changed fast. By early 2021, the CDC, American College of Chest Physicians, and Anticoagulation Forum all agreed: Don’t delay vaccines. The risk of getting sick far outweighs the small chance of a bruise.
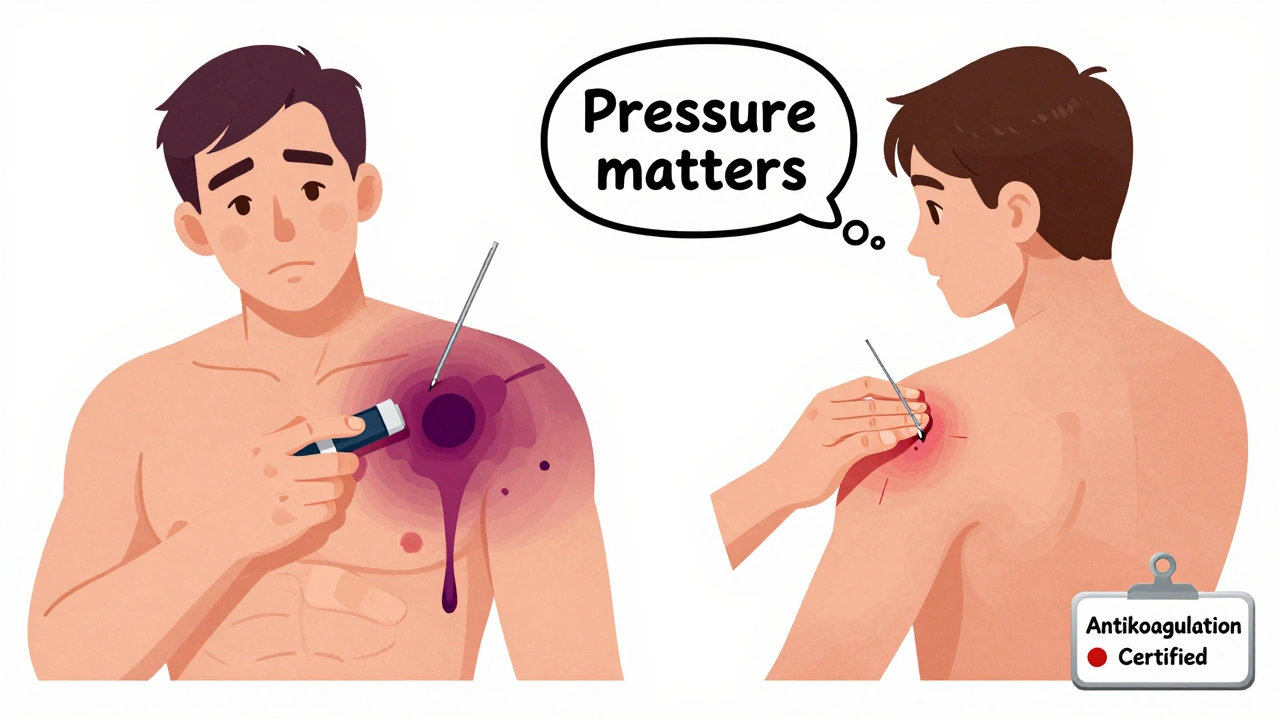
Injection Technique: The Real Game-Changer
How the shot is given matters more than the drug you take. Here’s what works:- Use a small needle. A 23-gauge or smaller needle causes less tissue damage. Most clinics use 25-gauge for adults-it’s thin enough to reduce bleeding risk.
- Inject into the deltoid muscle. The upper arm is the standard spot. Avoid the thigh unless you’re under 18 or have other reasons. The deltoid has less major blood flow than the thigh.
- Apply firm pressure for at least 10 minutes. This is the most overlooked step. Don’t just press. Don’t rub. Press straight down with your thumb or a clean gauze pad. Keep it steady. Ten minutes is the gold standard for people on blood thinners. Some guidelines say 2-5 minutes, but if you’re on warfarin or have had bruising before, go longer.
- No rubbing. Rubbing spreads the blood under the skin. That makes the bruise bigger. Just hold pressure. Count to 600 if you have to.
One patient on Reddit shared: “My nurse used a 25-gauge needle and held pressure for 10 minutes. No bruise. My last shot? They jabbed me, gave me a Band-Aid, and I had a purple lump the size of a golf ball.”
Warfarin vs. DOACs: Different Rules
Not all blood thinners are the same. Your approach depends on what you take.Warfarin (Coumadin) requires checking your INR before vaccination. The target range is usually 2.0-3.0. If your INR is above 4.0, you’re at higher risk for bleeding. Some doctors will delay the shot until your INR drops. Others will still give it but apply pressure for 10-15 minutes. The American Society of Hematology found patients with INR over 4.0 had a 37% higher chance of major bruising.
DOACs (rivaroxaban, apixaban, dabigatran, edoxaban) don’t need routine blood tests. You don’t need to check levels before vaccination. But timing matters. If you take apixaban twice daily, get the shot right after your morning dose. That way, the drug is at its lowest level in your blood. Same with rivaroxaban-give it after your daily dose. This isn’t about stopping the drug. It’s about reducing the peak concentration at the time of injection.
There’s no need to skip your dose. Stopping even for a day can increase your risk of stroke or clot. That’s far more dangerous than a bruise.
What About Those Weird Drug Interactions?
Back in 2004, a report from New Zealand mentioned rare cases where flu shots seemed to raise warfarin levels. One woman’s INR jumped from 2.8 to 8.1 after vaccination. But that’s been seen in fewer than 10 cases total since then. No such link has been found with DOACs.Modern research, including a 2024 study in Frontiers in Pharmacology, confirms that DOACs don’t interact with vaccines. Warfarin might have a tiny interaction in rare cases-but it’s not predictable. If you’re on warfarin and get a flu shot, check your INR in 7-10 days. Just to be safe. Most people see no change.
Don’t confuse this with drug interactions from new medications. If you start a new antibiotic or painkiller after your vaccine, that’s when you need to watch. Some drugs, like trimethoprim or amiodarone, can make warfarin stronger. But the vaccine itself? Not the issue.
What If You’re on Blood Thinners and Have Hemophilia?
If you have severe hemophilia (Factor VIII or IX under 1%), this is different. You’re not just on a blood thinner-you’re missing a key clotting protein. In this case, you need prophylactic treatment before the shot. Your hematologist will give you a dose of clotting factor 30-60 minutes before vaccination. This isn’t optional. Skipping it can cause serious bleeding into muscles or joints.For mild hemophilia, standard pressure techniques usually work. But always talk to your specialist. Don’t assume your primary care provider knows your full bleeding risk.
What Patients Say: Real Stories
A 2023 survey by the National Blood Clot Alliance polled 512 people on anticoagulants. Here’s what they found:- 68% had minor bruising after vaccines.
- 12% had large hematomas that needed medical care.
- 29% said their provider didn’t change technique for their blood thinner.
- Those with poor technique had 63% more complications.
One woman on HealthUnlocked wrote: “I’ve had five shots since starting Xarelto. Only one nurse knew to hold pressure. That’s the only one without a bruise.”
Another man on Reddit said: “I told my pharmacist I was on Eliquis. She said, ‘Oh, that’s fine.’ Then she jabbed me and walked away. I had a black eye on my arm for three weeks.”
These aren’t rare. They’re preventable.

What You Can Do Before Your Appointment
You’re not powerless. Here’s how to protect yourself:- Bring a list. Write down your medication, dose, and when you take it. Don’t rely on memory.
- Ask if they know the protocol. Say: “I’m on a blood thinner. Do you apply pressure for 10 minutes after shots?”
- Wear a wristband. Some clinics, like UCLA Health, now offer “Blood Thinner Alert” bands. Ask if yours does. If not, make your own with a Sharpie.
- Don’t be shy. If you’ve had a bad reaction before, say so. “I got a big bruise last time. Can we do something different?”
Many providers just don’t know the guidelines. A 2023 survey found only 87% of hospitals had formal protocols for anticoagulated patients. That means 13% still wing it. Don’t let that be you.
What to Watch After the Shot
Most bruising is harmless. But call your doctor if you notice:- Swelling that keeps growing after 24 hours
- Pain that gets worse instead of better
- Numbness or tingling in your arm
- Difficulty moving your shoulder
These could mean bleeding into deeper tissue or nerve compression. Rare, but serious.
For normal bruising, use ice for the first 24 hours. Then switch to heat. Avoid heavy lifting or strenuous arm use for a day. Don’t take aspirin or ibuprofen unless your doctor says it’s okay-they can make bleeding worse.
Bottom Line: Get the Shot. Do It Right.
You don’t have to choose between safety and protection. You can have both. Vaccines are essential. Bruises are avoidable. The science is clear: proper technique cuts complications by 78%, according to the Anticoagulation Forum.Don’t let fear stop you. But don’t let ignorance hurt you. Know your meds. Know your risks. Speak up. Ask for pressure. Demand the right needle. You’ve earned the right to be protected-not just from disease, but from preventable harm.
Can I still get vaccinated if my INR is high?
Yes, but with extra care. If your INR is above 4.0, the risk of bruising increases. Your provider may still give the shot but will apply firm pressure for 10-15 minutes. Some doctors prefer to wait until your INR is in the therapeutic range (usually 2.0-3.0), but delaying the vaccine is rarely necessary. The risk of getting the flu, pneumonia, or COVID-19 is far greater than the risk of a bruise.
Should I stop my blood thinner before a vaccine?
Never stop your blood thinner without talking to your doctor. Stopping even for a day can raise your risk of stroke, heart attack, or blood clots. The goal is not to stop the medication-it’s to adjust how the shot is given. Use a small needle, apply firm pressure for 10 minutes, and don’t rub the area. That’s all you need.
Do DOACs like Xarelto or Eliquis need special handling?
No blood tests are needed before vaccination with DOACs. But timing helps. Take your dose after the shot if you’re on once-daily apixaban or rivaroxaban. This lowers the drug level in your blood during the injection. Don’t skip your dose. The risk of a clot is much higher than the risk of a small bruise. Just make sure pressure is applied for at least 10 minutes.
Why do some people get huge bruises and others don’t?
It’s mostly about technique. People who get large hematomas often had the shot given too fast, with a large needle, or without enough pressure. Some providers don’t know the guidelines. Others rush. If you’ve had a bad experience before, speak up. Say, “I had a big bruise last time. Can we use a smaller needle and hold pressure longer?” That simple request can make all the difference.
Can I use a bandage or ice after the shot?
Yes, but only after applying firm pressure for 10 minutes. Don’t cover the site right away. Let the pressure do its job. After that, you can apply an ice pack for 15-20 minutes to reduce swelling. Avoid heat for the first 24 hours. After that, warm compresses can help the bruise fade. Never rub the area. And don’t take NSAIDs like ibuprofen unless your doctor says it’s safe-they can make bleeding worse.
If you’re on blood thinners, your next vaccine shouldn’t be a gamble. It should be a controlled, safe procedure. You’ve done the hard part by managing your condition. Now make sure your care team does theirs.

Annie Gardiner
December 7, 2025 AT 02:26Okay but have you ever considered that maybe vaccines are just a way to keep us docile? I mean, why do they always pick the deltoid? It’s right over the brachial plexus… coincidence? I think not. Also, I got a bruise the size of a small planet after my last shot and my cat started acting weird the next day. Coincidence? I think not.
Rashmi Gupta
December 8, 2025 AT 22:03Interesting. In India, we’ve been getting shots for decades without any of this fuss. No 10-minute pressure. No 25-gauge needles. Just jab and go. And yet, our elders live to 90. Maybe the problem isn’t the blood thinner… it’s the fear.
Andrew Frazier
December 10, 2025 AT 05:24Ugh. Another liberal vaccine pamphlet. Look, if you're on blood thinners, you're already one step away from the ER. Why not just stay home and pray? Also, 'DOACs'? That's just Big Pharma's way of charging you $500 for aspirin with a fancy name. And don't get me started on 'pressure for 10 minutes'-sounds like a yoga class, not a vaccine.
Mayur Panchamia
December 11, 2025 AT 22:52ABSOLUTELY! This is why India must lead the world in vaccine innovation! We don't need 25-gauge needles-we need 10-gauge needles with laser-guided precision and divine intervention! Also, why are we still using Western protocols? We have Ayurvedic hemostatic herbs that have been used since the Vedas! Why are we outsourcing common sense to America?!
brenda olvera
December 12, 2025 AT 22:33Y’all are overthinking this so hard lol. I’m on Xarelto and I just tell the nurse ‘hey, I’m on blood thinners, can we do the thing with the pressure?’ and they always do it. No drama. No trauma. Just kindness. You got this. You’re not broken. You’re just… well-informed. 💪
olive ashley
December 13, 2025 AT 12:49Wait… so you’re telling me the CDC and the American College of Chest Physicians are telling us to get vaccinated… but the same people who told us hydroxychloroquine was a miracle cure… and 5G caused COVID… and that masks were useless… are now the experts? I’m sorry. I don’t trust institutions that change their minds like a teenager changing outfits. This is a distraction. The real danger is the adjuvants. And the microchips. And the fact that they never tell you what’s *really* in the syringe.
Chris Park
December 15, 2025 AT 08:27It's fascinating how Western medicine has turned a simple intramuscular injection into a bureaucratic nightmare. In Nigeria, we have a saying: 'If you fear the needle, you fear life.' No pressure. No INR checks. No 10-minute vigil. Just the needle, the shot, and faith. The real problem isn't the blood thinner-it's the anxiety engineered by pharmaceutical marketing departments. You're being manipulated into believing you're fragile. You're not.
Nigel ntini
December 17, 2025 AT 03:30This is exactly the kind of clear, practical advice we need more of. So many people are scared to speak up-but you’ve laid it out so simply: small needle, firm pressure, no rubbing. That’s it. And to those who say ‘I’ve never heard of this’-tell your provider. They’re human too. They want you to be safe. You’re not being difficult. You’re being smart. Keep advocating. You’re not alone.
Mansi Bansal
December 18, 2025 AT 10:01It is with profound concern that I observe the casual dismissal of medical protocols in this discourse. The administration of vaccines to individuals on anticoagulant therapy constitutes a high-risk medical procedure requiring standardized, institutionalized oversight. To reduce it to a matter of 'pressing for ten minutes' is to trivialize the physiological complexity of hemostasis. One must consider the pharmacokinetic half-lives, the fibrinolytic cascade, and the potential for subclinical hemorrhage. This is not a matter of patient preference-it is a matter of bioethical obligation.
pallavi khushwani
December 19, 2025 AT 06:48i just think it’s wild that we’ve turned something so simple into this whole thing. like, yeah, bruising sucks. but we’ve been getting shots forever. maybe the real issue is that we’ve forgotten how to trust our bodies? or the people giving us shots? just breathe. ask nicely. let them know. most nurses want to do right by you. it’s not a battle. it’s a moment.
Dan Cole
December 20, 2025 AT 15:09Let me break this down for you with the precision of a neurosurgeon: The entire premise of this article is flawed because it assumes that 'pressure' is the solution. But pressure doesn't stop bleeding-it only delays it. The real solution is to administer the vaccine intravenously in a controlled setting, bypassing the capillary bed entirely. Also, did you know that the deltoid is the only muscle with a direct neural connection to the vagus nerve? That's why you get fainting spells. This isn't about bruising-it's about autonomic sabotage. The CDC is hiding this.
Billy Schimmel
December 22, 2025 AT 08:30Wow. So basically, if you're on blood thinners, you're just supposed to be the annoying person who makes the nurse pause and think for 10 seconds? And that’s the whole secret? I’m impressed. I thought it was magic. Turns out it’s just… being polite and not a jerk. Who knew?
Shayne Smith
December 23, 2025 AT 22:38My nurse didn’t know any of this. I had to teach her. She was nice about it. We both laughed. Then she held pressure for 12 minutes. No bruise. I brought cookies next time. She remembered me. Small wins.
Max Manoles
December 25, 2025 AT 05:13One thing this article doesn’t mention: the psychological toll of being the person who ‘needs special treatment.’ I’ve had nurses sigh when I say I’m on Eliquis. I’ve been asked if I’m ‘that guy’ who always complains. I don’t want to be that guy. I just want to live. Maybe the real solution isn’t in needles or pressure-it’s in systemic change. Training. Standardization. A culture where asking for safety isn’t seen as a burden, but as a right.