Fournier's Gangrene Risk Assessment Tool
Important Safety Information
Time is tissue. Time is life. Fournier's gangrene is a medical emergency. If you experience ANY of the symptoms below, go to the emergency room immediately.
Risk Factors Assessment
Check all factors that apply to your situation. Each factor adds risk. This tool estimates your relative risk but does NOT replace medical advice.
Your Risk Assessment
CRITICAL ACTION REQUIRED
Based on your risk factors, if you experience ANY of the following symptoms:
- Severe pain in genital/anal area
- Redness, swelling, or discoloration
- Fever or chills
- Foul-smelling discharge
GO TO EMERGENCY ROOM IMMEDIATELY. Every hour counts. Time is tissue.
Recommended Steps:
- Stop taking SGLT2 inhibitor immediately
- Call emergency services or go to ER
- Do NOT wait for doctor appointment
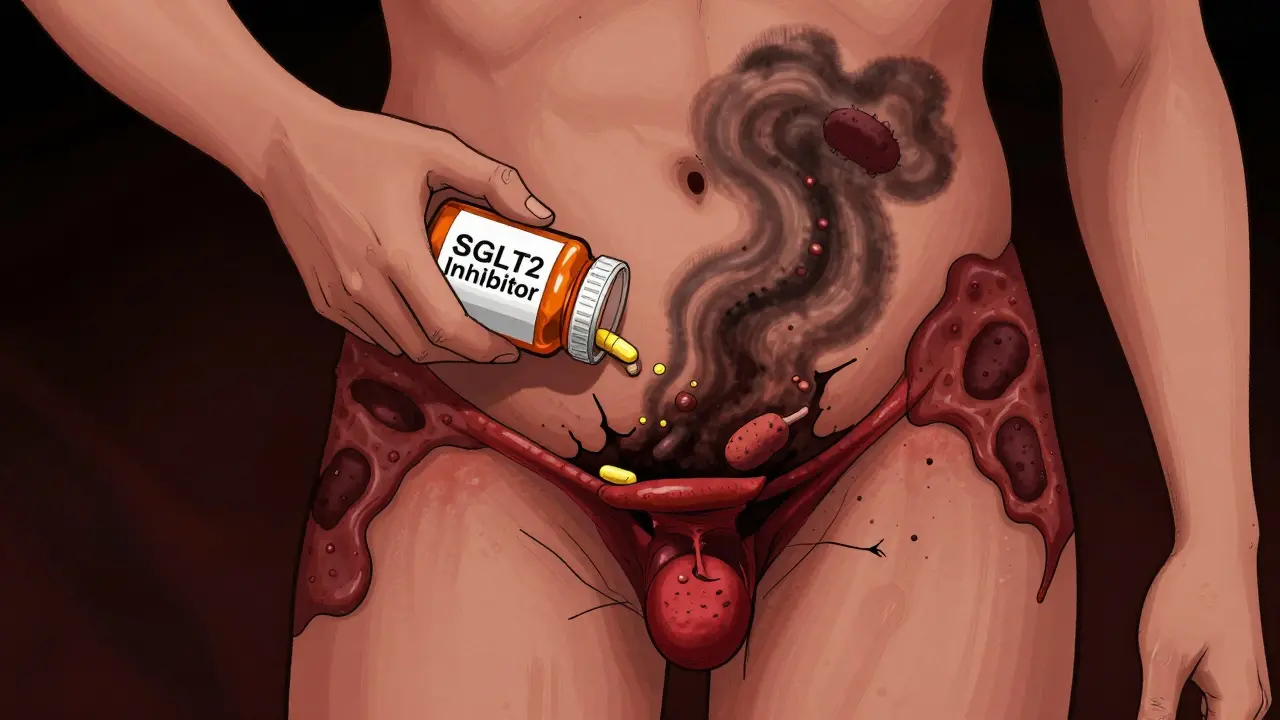
When you’re managing type 2 diabetes, the goal is simple: keep your blood sugar stable and protect your heart and kidneys. SGLT2 inhibitors like canagliflozin, a sodium-glucose cotransporter-2 inhibitor used to lower blood sugar by making the kidneys remove excess glucose through urine, dapagliflozin, another SGLT2 inhibitor approved in 2014 that reduces cardiovascular events in high-risk patients, empagliflozin, a drug shown in trials to cut heart failure hospitalizations by 35% in people with diabetes and heart disease, and ertugliflozin, a newer SGLT2 inhibitor with limited long-term safety data have become go-to medications because they do more than just lower glucose. They reduce heart failure, slow kidney disease, and help with weight loss. But there’s one rare, terrifying complication you must know about: Fournier’s gangrene, a rapidly spreading, life-threatening bacterial infection that destroys skin, fat, and tissue in the genital and anal areas.
What Is Fournier’s Gangrene - And Why Should You Care?
Fournier’s gangrene isn’t something you hear about often. It’s not a common cold or a rash. It’s a medical emergency. Bacteria - often a mix of E. coli, staph, and anaerobic bugs - invade the skin and fat around your genitals or anus. They spread fast. Within hours, tissue dies. The area turns black, swells up, and becomes excruciatingly painful. Fever, chills, and a feeling of being utterly sick follow. If you wait too long, the infection enters your bloodstream. Sepsis kicks in. Death can happen in under 48 hours. This isn’t just a risk for people with weak immune systems. It’s happened to otherwise healthy men and women taking SGLT2 inhibitors. Between 2013 and 2018, the FDA confirmed 12 cases. By 2024, that number had grown. The UK reported six cases linked to these drugs up to early 2019. One in 10,000 men on these medications might develop it. That sounds tiny. But when the alternative is death, even one case is too many.How Do SGLT2 Inhibitors Lead to This?
SGLT2 inhibitors work by telling your kidneys to dump sugar into your urine. That’s great for lowering blood sugar. But it also means your urine is full of glucose - sugar. And sugar is food for bacteria. Think about it: every time you pee, you’re leaving a sweet, warm, moist environment right around your genitals. That’s a perfect breeding ground. The sugar doesn’t just feed bacteria - it can weaken your skin’s natural defenses. Your body’s ability to fight off infection gets dampened. Add in poor blood sugar control, which many people with diabetes struggle with, and you’ve got a perfect storm. Studies show that nearly all reported cases involved people with HbA1c levels above 9%. That’s not just high - it’s dangerously high. So while the drug plays a role, uncontrolled diabetes is the silent partner in this deadly combo.Early Warning Signs You Can’t Ignore
The biggest mistake people make? Waiting. They think it’s a yeast infection. Or a pimple. Or a pulled muscle. It’s not. If you’re taking any SGLT2 inhibitor and you notice any of these symptoms - even if they seem mild - act immediately:- Severe pain in your genitals, anus, or perineum (the area between them)
- Redness, swelling, or warmth that spreads quickly
- Dark or discolored skin - black, purple, or gray patches
- Fever, chills, or feeling extremely unwell
- Foul-smelling discharge from the genital area
- Difficulty urinating or pain while peeing

What to Do If You Suspect Fournier’s Gangrene
Time is tissue. Time is life. Step 1: Stop the SGLT2 inhibitor immediately. Don’t wait for a doctor’s call. Don’t check your email. Don’t wait until morning. Take the pill out of your routine right now. This isn’t optional. Step 2: Go to the ER. Now. Call ahead if you can. Say: “I’m on an SGLT2 inhibitor and I think I might have Fournier’s gangrene.” Emergency rooms know this risk. They’ve been warned. They’ll prioritize you. Step 3: Expect urgent treatment. You’ll get broad-spectrum antibiotics - likely a mix of drugs to kill multiple types of bacteria. You’ll need surgery. Not tomorrow. Not in two days. Within hours. Surgeons will cut away dead tissue to stop the infection from spreading. This is brutal, but it’s the only way to survive. Every hour you delay increases your risk of death by about 9%. That’s not a guess. That’s from studies of over 200 cases. If you’re treated within 24 hours, your chance of survival is over 80%. After 48 hours? It drops below 50%.Who’s at Higher Risk?
You might think this only affects men. It doesn’t. While 70% of cases are in men, nearly one-third of reported cases in Europe were in women. That’s not a footnote - it’s a warning. You’re at higher risk if:- Your HbA1c is above 9%
- You’ve had recurrent genital yeast infections (thrush) in the past year
- You have a weakened immune system (from steroids, chemotherapy, or autoimmune disease)
- You’re overweight or have poor hygiene
- You have diabetes for more than 10 years
Should You Stop Taking Your SGLT2 Inhibitor?
No - not unless you have symptoms. These drugs save lives. They cut heart failure hospitalizations. They protect your kidneys. For most people, the benefits far outweigh the risk. The FDA, the European Medicines Agency, and the UK’s MHRA all say the same thing: Don’t stop. But stay alert. The risk isn’t zero. But it’s extremely low. One extra case per 10,000 people treated. That’s less than the risk of a car accident on a short commute. But unlike a car crash, this one has a clear warning sign - and you can act on it.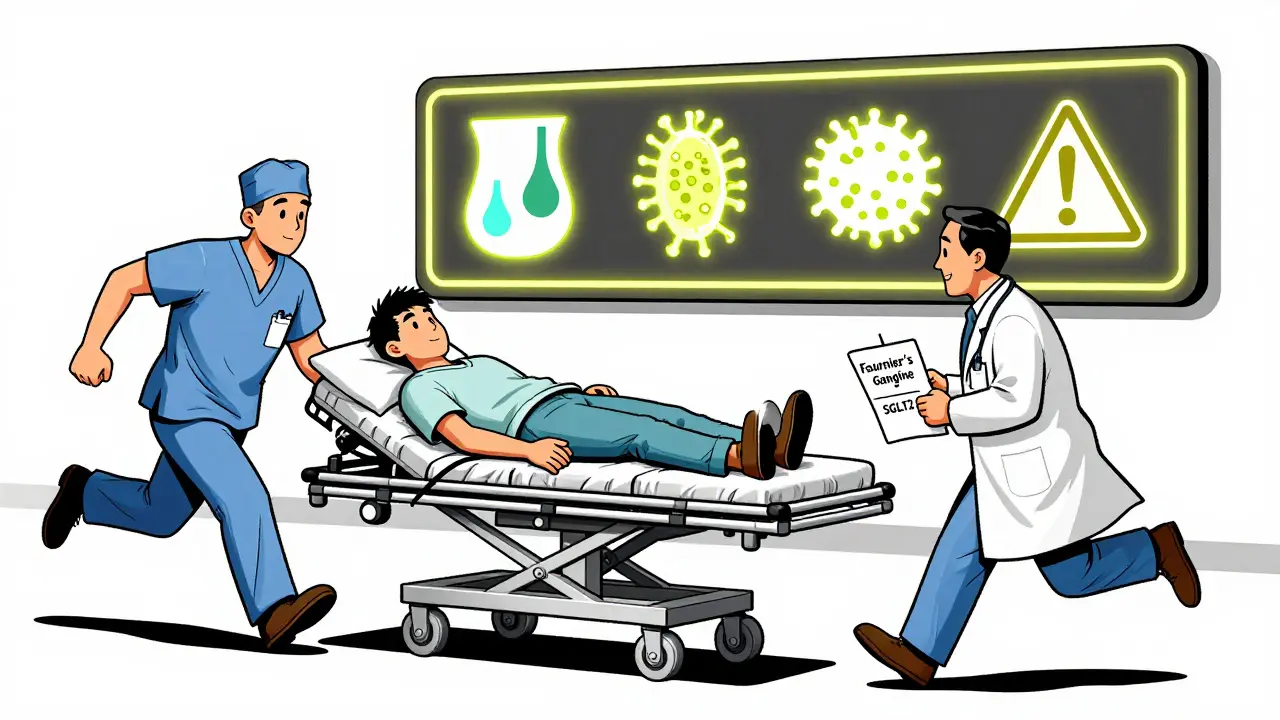
What Your Doctor Should Tell You
When you’re prescribed an SGLT2 inhibitor, your doctor should explain this risk - clearly. Not as a footnote. Not as a generic “watch for infections.” But specifically:- “This drug increases glucose in your urine.”
- “That can lead to a rare but deadly infection in your genital area.”
- “If you feel sudden, severe pain, swelling, or discoloration - go to the ER immediately.”
- “Do not wait. Do not call me first. Go to the hospital.”
The Bigger Picture
This isn’t about scaring you off SGLT2 inhibitors. It’s about empowering you. These drugs are among the most important advances in diabetes care in decades. But they’re not magic. They work best when you’re informed. If you’re on one, keep your blood sugar under control. Monitor your genital area. Shower regularly. Keep the area dry. Don’t ignore odd sensations. And if something feels wrong - don’t wait. Don’t hope it’s nothing. Go.FAQ
Can women get Fournier’s gangrene from SGLT2 inhibitors?
Yes. While most cases occur in men, about one-third of reported cases in Europe involved women. The mechanism - glucose in urine creating a bacterial breeding ground - applies to anyone with a genital area. Women should be just as vigilant about sudden pain, swelling, or discoloration in the genital or perineal region.
Is Fournier’s gangrene contagious?
No. Fournier’s gangrene is not contagious. You can’t catch it from someone else. It’s caused by bacteria already in your body - often from your gut - that spread into the skin and tissue. The SGLT2 inhibitor doesn’t introduce new bacteria; it creates conditions that let your own bacteria turn dangerous.
Can I switch to another diabetes drug if I’m worried?
Yes. If you’re concerned, talk to your doctor. Alternatives include GLP-1 receptor agonists (like semaglutide or liraglutide), metformin, or DPP-4 inhibitors. These don’t carry the same risk of Fournier’s gangrene. But don’t stop your current medication without medical advice - uncontrolled diabetes is far more dangerous than the rare risk of this infection.
How long after starting an SGLT2 inhibitor can Fournier’s gangrene develop?
It can happen anytime after starting the drug - even years later. Most cases occur within the first 6 to 12 months, but reports exist up to 5 years after starting. There’s no safe time window. That’s why ongoing awareness matters, not just during the first few weeks.
Are all SGLT2 inhibitors equally risky?
Yes. The risk appears to be a class effect - meaning all drugs in this group carry the same potential risk. Canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin are all linked to cases. It’s not one bad apple - it’s how the whole class works. If you’ve had a reaction with one, switching to another won’t help.