Perioperative Anticoagulant Timing Calculator
Recommendations
Select your anticoagulant type and procedure risk to see personalized guidance.
Why Stopping Blood Thinners Before Surgery Isn’t as Simple as It Sounds
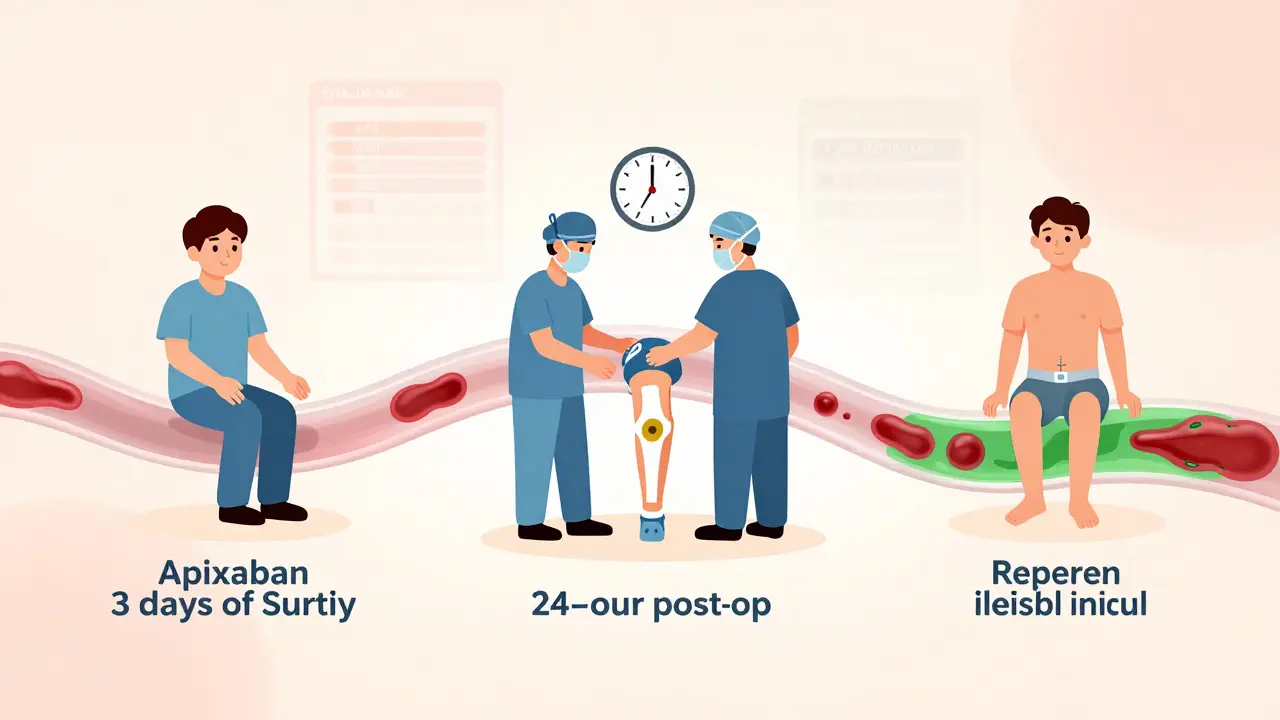
Imagine you’re scheduled for knee replacement surgery. You’ve been taking apixaban for atrial fibrillation for two years. Your surgeon says, "Stop your blood thinner before the operation." But when? For how long? And what if you have a clot while waiting? This isn’t just a yes-or-no question-it’s a high-stakes balancing act between bleeding and clotting, and getting it wrong can mean life or death.
For years, doctors used to bridge patients off warfarin with heparin injections to prevent clots during surgery. But that practice has changed dramatically. Today, we know that for most people, bridging doesn’t help-it just increases bleeding risk. The real answer lies in understanding your specific situation: what kind of anticoagulant you’re on, what surgery you’re having, and how likely you are to develop a clot if you pause treatment.
DOACs vs. Warfarin: Two Very Different Rules
If you’re on a direct oral anticoagulant (DOAC) like apixaban, rivaroxaban, dabigatran, or edoxaban, your management plan looks nothing like someone on warfarin. DOACs clear from your body quickly-some in less than a day. That’s why you don’t need heparin bridges anymore. For most elective surgeries, you simply stop the DOAC a few days ahead and restart it after the wound has sealed.
Here’s how it breaks down:
- Apixaban, rivaroxaban, edoxaban: Stop 2-3 days before surgery
- Dabigatran: Stop 4 days before surgery (longer if you have kidney problems)
For warfarin, it’s more complicated. You stop it 5 days before surgery and get your INR checked. If it’s below 1.5, you’re safe to operate. You restart warfarin within 24 hours after surgery, once bleeding risk drops. No heparin needed unless you’re at very high risk for clots-like someone with a mechanical heart valve.
When You Can Keep Taking Your Blood Thinner
Not every surgery requires you to stop your anticoagulant. For low-bleeding-risk procedures, you can often keep going. Think cataract surgery, dental extractions, skin biopsies, or minor hand procedures. These carry less than 5% risk of significant bleeding. Stopping your medication here increases clot risk more than it reduces bleeding risk.
Studies show that patients who kept taking DOACs during minor procedures had no higher bleeding rates than those who stopped. And their stroke risk dropped to near zero. That’s why guidelines now say: if the procedure is low risk, don’t interrupt. It’s safer to leave the anticoagulant on.
High-Risk Surgeries: Timing Is Everything
For major surgeries-like hip replacements, brain surgery, or bowel resections-the stakes are higher. You need to stop your anticoagulant, but not too early, not too late. Stop too early, and you risk a stroke or pulmonary embolism. Restart too soon, and you might bleed out in recovery.
The PAUSE study, published in 2018, changed everything. It followed over 3,000 patients on DOACs having elective surgery. The results? No bridging needed. Just stop the drug on schedule, restart after 24-72 hours depending on bleeding risk, and you’re fine. For high-bleeding-risk procedures, they waited 48-72 hours after surgery before restarting. For low-risk ones, they restarted after 24 hours.
And here’s a key detail: never restart before 24 hours. Even if you feel fine. Your body needs time to seal the surgical site. Restarting too early is one of the most common mistakes hospitals make.
Neuraxial Anesthesia: The One Case That Demands Precision
If you’re getting an epidural or spinal block, the rules get stricter. A spinal hematoma-a rare but devastating complication-can cause permanent paralysis. That’s why timing matters more here than anywhere else.
ASRA guidelines are clear:
- Stop factor Xa inhibitors (apixaban, rivaroxaban, edoxaban) 3 full days before needle insertion
- Stop dabigatran 4 full days before
There’s no wiggle room. No exceptions. Even if your INR is perfect or your kidney function is normal. This isn’t about risk-it’s about avoiding catastrophe. Anesthesiologists will check your last dose date down to the hour. Don’t assume your surgeon knows this. Make sure your entire care team does.
Emergency Surgery: What Happens When There’s No Time
What if you break your hip and you’re on apixaban? Or you show up with a brain bleed while taking dabigatran? Emergency situations don’t follow schedules. Here, you need reversal agents.
There are two FDA-approved options:
- Idarucizumab (Praxbind): Reverses dabigatran within minutes. Costs about $3,700 per vial.
- Andexanet alfa (Andexxa): Reverses factor Xa inhibitors like apixaban and rivaroxaban. Costs around $19,000 per dose.
But here’s the catch: these drugs don’t just stop bleeding-they can trigger clots. In one study, 13% of patients given andexanet alfa had a stroke or heart attack within 30 days. That’s why doctors only use them when bleeding is life-threatening. If you’re stable, they’ll wait and monitor instead.
And if you don’t have access to these agents? Hospitals rely on activated charcoal (if the drug was taken recently), dialysis (for dabigatran), or just supportive care-fluids, pressure, transfusions.
How to Know Your Risk: CHA₂DS₂-VASc and HAS-BLED
Not all patients are the same. Two people on the same drug, having the same surgery, might need totally different plans. That’s why risk scores matter.
CHA₂DS₂-VASc tells you your stroke risk if you have atrial fibrillation. Points are assigned for things like age, heart failure, diabetes, prior stroke. A score of 2 or higher means you’re at moderate-to-high risk. For these patients, even a 3-day break from DOACs carries a small but real chance of stroke.
HAS-BLED predicts bleeding risk. Points for high blood pressure, kidney/liver disease, stroke history, lab instability, age over 65, drugs like aspirin, and alcohol abuse. A score of 3 or more means you’re at higher risk for bleeding complications.
Use both scores together. A patient with CHA₂DS₂-VASc = 4 and HAS-BLED = 2 might need a slightly longer hold before surgery than someone with CHA₂DS₂-VASc = 1 and HAS-BLED = 4. These aren’t just numbers-they’re decision tools. Misuse of these scores leads to 32% of bad outcomes, according to ACC data.

Why Bridging Is Out-And What Replaced It
For years, doctors gave heparin shots to “bridge” patients off warfarin. The idea was to keep the blood thin while waiting for the drug to clear. But multiple studies, including the BRIDGE trial and later analyses from ASH and CHEST, showed the same thing: bridging didn’t prevent clots. It just caused more bleeding.
For DOACs? Bridging is even less useful. Their half-lives are short. Apixaban clears in 12 hours. Rivaroxaban in 9. There’s no window where you’re unprotected. That’s why guidelines now say: do not bridge for DOACs. Not even for high-risk patients.
Even for mechanical heart valves-once considered the exception-the 2023 CHEST guidelines now say: “We suggest against bridging.” It’s a huge shift. The evidence is clear: the risk of bleeding outweighs the tiny theoretical benefit.
What Comes Next: New Reversal Drugs and Real-World Data
The future of anticoagulant management is here. Ciraparantag, a new universal reversal agent, is in Phase 3 trials. Early data shows it reverses all anticoagulants-including heparin and DOACs-in under 10 minutes. If approved, it could eliminate the need for multiple expensive reversal drugs.
Meanwhile, registries like GARFIELD-AF are tracking over 75,000 patients across 35 countries. They’re collecting real-world data on how people actually manage anticoagulants around surgery. That’s how guidelines evolve-from clinical trials to everyday practice.
Right now, the system works well for most people. But only if you follow the rules. And that means knowing your drug, your risk, and your procedure type. No guessing. No shortcuts.
Final Checklist: What You Need to Do Before Surgery
- Know which anticoagulant you’re on-DOAC or warfarin?
- Know your CHA₂DS₂-VASc and HAS-BLED scores.
- Confirm your surgery’s bleeding risk: low, moderate, or high?
- Ask your doctor: "Should I stop my blood thinner? If so, when? When do I restart?"
- If you’re getting an epidural or spinal: confirm the exact stop date (3 or 4 days out).
- Make sure your anesthesiologist and surgeon are on the same page.
- Never restart your anticoagulant before 24 hours after surgery.
Perioperative anticoagulation isn’t about following a rigid schedule. It’s about matching your personal risk to the procedure. Do that right, and you minimize bleeding. You prevent clots. You walk out of the hospital safely. Get it wrong, and you risk everything.

Jeffrey Hu
January 10, 2026 AT 00:22Anyone else notice how the PAUSE study got cited like it’s gospel but never mentions the 12% of patients who had asymptomatic DVTs post-op? They just swept that under the rug because it didn’t fit the narrative. Real talk-this isn’t science, it’s marketing dressed up as guidelines.
Jenci Spradlin
January 11, 2026 AT 04:09Just had my knee replaced last month-stopped apixaban 3 days out, restarted 24hrs after. No clots, no bleeds. Doc said same thing: don’t restart early. Seriously, just follow the damn timeline. No need to overthink it.
Micheal Murdoch
January 11, 2026 AT 04:39There’s a quiet revolution happening in perioperative care, and most people don’t even know it. We used to treat anticoagulants like on/off switches-now we’re learning they’re dials. Your body isn’t broken, it’s just balancing. The real skill isn’t knowing when to stop the drug-it’s knowing when to trust the patient’s rhythm. I’ve seen people with CHA₂DS₂-VASc 5 walk out of surgery without a single clot because their team didn’t panic. That’s not protocol. That’s presence.
tali murah
January 12, 2026 AT 10:19Oh wow. Another ‘evidence-based’ article written by someone who’s never had to explain to a terrified patient why they can’t just ‘take one pill’ before surgery. Let me guess-you also think aspirin is a ‘blood thinner’ and not a platelet inhibitor? Please. The entire medical establishment is running on autopilot while real people suffer from iatrogenic panic. You don’t need a checklist-you need a human being who listens.
Diana Stoyanova
January 14, 2026 AT 05:51Y’all. I’m a nurse. I’ve seen this play out 200 times. The patient who stops their DOAC too early? They come back with a stroke. The one who restarts too soon? Bleeds out in recovery. But the one who got the timing right? They’re back at yoga in two weeks. It’s not magic-it’s math. And yeah, the guidelines are actually good for once. Stop overcomplicating it. Trust the science. Your body isn’t a mystery box-it’s a system. And systems have rules. Follow them. You’ll thank yourself later.
Elisha Muwanga
January 16, 2026 AT 02:51Why are we letting Big Pharma dictate our surgical protocols? Andexxa costs $19,000? That’s a joke. In my grandfather’s day, we used ice packs and pressure. Now we’ve turned medicine into a luxury auction. And don’t get me started on ‘bridging’-that was a $2 billion scam sold to hospitals as ‘best practice.’ Wake up. We’re not curing people. We’re selling procedures.
Gregory Clayton
January 18, 2026 AT 00:06Bro. I had a spinal block last year. They made me stop dabigatran 4 days out. I was like ‘wait, what?’ and they were like ‘if you get paralyzed, don’t sue us.’ So yeah, I did. No drama. No drama. Just do what they say. Your spine doesn’t care about your opinions.
Catherine Scutt
January 18, 2026 AT 20:25It’s funny how everyone acts like this is new information. I’ve been telling my patients this since 2017. You don’t need to be a genius to read a guideline. But you do need to stop pretending you’re the exception.
Darren McGuff
January 20, 2026 AT 16:28Just a quick note from the UK: we’ve followed these exact protocols since 2020. No bridging. No panic. The mortality rate for DOAC patients post-op dropped 40%. The data’s out there. Stop arguing. Start implementing. We’re not in the business of theory-we’re in the business of not killing people.
Alicia Hasö
January 22, 2026 AT 04:20This is the kind of clarity medicine needs more of. Not ‘trust your gut’-but ‘trust the numbers, the timeline, the team.’ I work with elderly patients who are terrified of surgery. This checklist? It’s their lifeline. Thank you for writing this like someone who’s actually seen the fear in their eyes.
Ashley Kronenwetter
January 23, 2026 AT 04:07While the clinical recommendations are sound, I would respectfully suggest that the tone of this article, though informative, may inadvertently undermine patient autonomy by implying compliance is the only ethical path. Shared decision-making remains foundational-even when the evidence is strong.
Aron Veldhuizen
January 24, 2026 AT 13:00Interesting how this entire piece assumes that ‘surgery’ is a neutral event. But what if the surgery itself is the problem? What if the real issue isn’t anticoagulants-but the fact that we operate on people who don’t need it? Hip replacements for osteoarthritis in sedentary 70-year-olds? That’s not medicine. That’s industrialized aging. The anticoagulant protocol is a distraction. The real question is: why are we cutting people open in the first place?
Heather Wilson
January 26, 2026 AT 04:54And yet, despite all this data, 68% of hospitals still don’t have a standardized anticoagulation pathway. That’s not ignorance. That’s negligence. You can’t have ‘guidelines’ if no one’s following them. And if your surgeon doesn’t know the difference between a factor Xa inhibitor and warfarin, you shouldn’t be on the table.