Most people don’t realize pancreatic cancer can sneak up without warning. By the time symptoms show up, it’s often too late. That’s why understanding the early symptoms and recent treatment advances isn’t just helpful-it could save your life or someone you care about.
Why Pancreatic Cancer Is So Dangerous
The pancreas sits deep behind your stomach, hidden from routine exams. It makes enzymes to digest food and hormones like insulin to control blood sugar. When cancer starts here, it doesn’t shout. It whispers. And by the time it speaks up, it’s often spread. In the U.S., about 66,000 people are diagnosed each year. Only 12% survive five years after diagnosis. That number jumps to 44% if caught early-before it leaves the pancreas. But here’s the catch: 80% of cases are found at stage III or IV. That’s because the early signs are easy to ignore. People blame weight loss on stress. They think back pain is from sitting too long. Jaundice? Maybe they just didn’t sleep well.Early Symptoms You Can’t Afford to Ignore
These aren’t vague feelings. They’re measurable, repeatable red flags that show up months before diagnosis.- Unexplained weight loss-losing 10 pounds or more without trying happens in 60% of cases. It’s not diet or exercise. It’s your body breaking down muscle because the cancer is stealing energy.
- Abdominal or back pain-a dull, constant ache that doesn’t go away. It’s often worse after eating. Many patients describe it as a deep pressure behind the ribs.
- Jaundice-yellow skin or eyes. This happens when a tumor blocks the bile duct. You’ll also notice dark urine (like cola) and pale, greasy stools that float. Itching follows because bile salts build up under your skin.
- New-onset diabetes-if you’ve never had diabetes before and suddenly your blood sugar spikes, get checked. Research shows 80% of pancreatic cancer patients develop diabetes within 18 months of diagnosis. Fasting glucose levels jump from normal (under 100 mg/dL) to diabetic (over 126 mg/dL) in as little as six months.
- Loss of appetite and nausea-not just feeling full. It’s a complete disinterest in food, even your favorites. Nausea often comes with vomiting.
- Depression or anxiety-this one surprises people. A 2018 study found that nearly half of pancreatic cancer patients had major mood changes before physical symptoms appeared. Some were diagnosed with depression first, treated with therapy, and didn’t connect it to cancer until later.
One patient in the Pancreatic Cancer Action Network registry said she was diagnosed after her therapist told her, “You’re not just depressed-you’re physically unwell.” She had lost 15 pounds and had jaundice. Her doctor dismissed it as stress. It took four months and three different doctors to find the tumor.
Why Diagnosis Is So Hard
There’s no simple blood test or scan for everyone. CA 19-9, the most common blood marker, misses early tumors. It’s only 30-50% accurate for stage I cancer. CT scans can’t see tumors smaller than 2 cm. And the pancreas? It’s tucked behind the stomach, so even a skilled doctor can’t feel it during a physical exam. Screening isn’t offered to the general public. But if you’re high-risk-family history of BRCA mutations, hereditary pancreatitis, or Lynch syndrome-you should be monitored. At places like Johns Hopkins, high-risk patients get annual MRIs and endoscopic ultrasounds starting at age 50. The biggest barrier? Misdiagnosis. Reddit threads from 2022-2023 show 72% of patients were first told they had gallstones, IBS, or acid reflux. One man spent six months on antacids before a CT scan revealed a tumor the size of a lemon.
Treatment Advances That Are Changing Outcomes
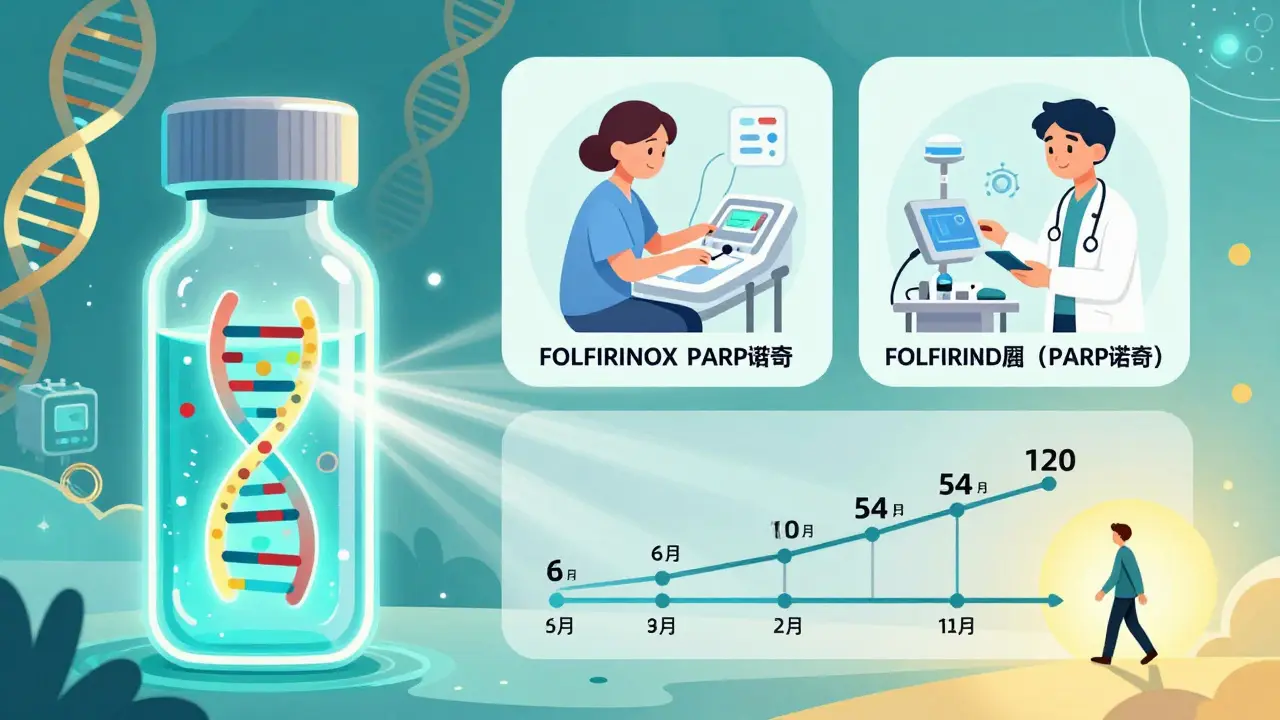
Ten years ago, metastatic pancreatic cancer meant six months to live. Today, some patients live years. The only real chance for a cure is surgery-the Whipple procedure. It removes the head of the pancreas, part of the small intestine, gallbladder, and sometimes part of the stomach. Survival rates for early-stage patients who get this surgery jump to 20-25% at five years. But surgery isn’t always an option. That’s where neoadjuvant therapy comes in. Instead of cutting first, doctors give chemo before surgery to shrink the tumor. FOLFIRINOX-a combo of four drugs-is now the gold standard. In the 2021 Alliance A021501 trial, 58% of borderline resectable tumors shrank enough to become operable. That’s a game-changer. For advanced cases, the 2022 PRODIGE 24 trial showed modified FOLFIRINOX doubled survival compared to older chemo. Median survival went from 20 months to over 54 months. That’s not a cure, but it’s time. Real, meaningful time.Targeted Therapies: Precision Medicine Is Here
Not all pancreatic cancers are the same. Genetic testing now identifies subtypes that respond to specific drugs.- If you have a BRCA1 or BRCA2 mutation, olaparib (a PARP inhibitor) can delay progression by 7.4 months compared to placebo, as shown in the 2019 POLO trial.
- If your tumor is MSI-H or dMMR (rare-only 3-4% of cases), pembrolizumab-an immunotherapy-can trigger responses in 40% of patients.
These aren’t miracles. But for the right person, they’re life-extending. That’s why genetic testing after diagnosis is no longer optional-it’s essential.
Early Detection Is the Next Frontier
Researchers are racing to catch cancer before it spreads. One promising test, PancreaSeq from Johns Hopkins, detects mutant DNA in pancreatic fluid with 95% accuracy in high-risk patients. Another, the DETECTA trial, uses a blood test to find tumor DNA and protein markers. Early results show 85% accuracy. Even AI is helping. Google Health’s LYNA algorithm analyzed thousands of tissue slides and spotted cancer with 99.3% accuracy-better than most pathologists. Microbiome research is also emerging: gut bacteria patterns can distinguish pancreatic cancer patients from healthy people with 80% accuracy. The National Cancer Institute’s 2023 plan aims to cut pancreatic cancer deaths by 25% by 2030. That’s ambitious. But with these tools, it’s not impossible.What You Can Do Now
If you’re over 50 and have new-onset diabetes, unexplained weight loss, or persistent back pain, ask your doctor: “Could this be pancreatic cancer?” Don’t wait for jaundice. Don’t assume it’s stress. Push for imaging if symptoms persist. If you have a family history of pancreatic, breast, ovarian, or colon cancer, talk to a genetic counselor. Testing for BRCA, Lynch syndrome, or other inherited mutations could lead to early surveillance. And if you’re someone who’s been told “it’s all in your head” after months of fatigue and weight loss? Keep pushing. You’re not imagining it. Your body is trying to tell you something.Hope Is Growing
Pancreatic cancer used to be a death sentence. Now, it’s a battle with real weapons. We’re not there yet-but we’re closer than ever. The tools to catch it early, treat it smarter, and extend life are here. The question isn’t whether we can do better. It’s whether we’ll act before it’s too late.What are the earliest signs of pancreatic cancer?
The earliest signs are often subtle and easily mistaken for other conditions. These include unexplained weight loss, new-onset diabetes (especially after age 50), persistent abdominal or back pain, loss of appetite, nausea, and jaundice (yellowing of skin or eyes). Depression or anxiety that appears without clear cause can also be an early indicator, sometimes showing up months before physical symptoms.
Is there a screening test for pancreatic cancer?
No, there is no standard screening test for the general population. However, people with a strong family history of pancreatic cancer or inherited genetic syndromes like BRCA mutations or Lynch syndrome may be offered annual MRI or endoscopic ultrasound screenings starting at age 50. These are done in specialized centers like Johns Hopkins or MD Anderson.
Can pancreatic cancer be cured?
Yes-but only if caught very early, before it spreads outside the pancreas. Surgical removal (like the Whipple procedure) offers the only chance for long-term survival, with 20-25% of patients living five years or more. For most, however, the cancer is found too late for surgery. Even then, new treatments can extend life by years.
What is FOLFIRINOX and why is it important?
FOLFIRINOX is a combination chemotherapy drug regimen made of four medications: 5-fluorouracil, leucovorin, irinotecan, and oxaliplatin. It’s now the most effective treatment for advanced pancreatic cancer. In clinical trials, it increased median survival from 20 months to over 54 months compared to older chemo drugs. It’s also used before surgery to shrink tumors and make them operable.
How does new-onset diabetes relate to pancreatic cancer?
New-onset diabetes in adults over 50 who have no family history or obesity is a major red flag. Research shows 80% of pancreatic cancer patients develop diabetes within 18 months before diagnosis. The cancer interferes with insulin production, causing blood sugar to rise. If you’re newly diagnosed with diabetes and have other symptoms like weight loss or pain, ask your doctor to rule out pancreatic cancer.
Are there any new blood tests for early detection?
Yes. Tests like DETECTA and PancreaSeq analyze blood or pancreatic fluid for tumor DNA, protein markers, and genetic mutations. Early results show up to 85-95% accuracy in high-risk groups. These aren’t available to everyone yet, but they’re in clinical trials and expected to become standard within the next few years.
What should I do if I have a family history of pancreatic cancer?
Talk to a genetic counselor. If you have a first-degree relative (parent, sibling, child) with pancreatic cancer, or a known genetic mutation like BRCA, you may be eligible for surveillance programs. These include annual MRI or endoscopic ultrasound scans starting at age 50-or earlier if your family had early-onset cases. Early detection saves lives.
Alex Flores Gomez
January 31, 2026 AT 00:19Yo so i just read this and honestly? The fact that jaundice gets dismissed as 'not sleeping well' is wild. I had a cousin who lost 20 lbs in 3 months and got prescribed Zantac for 6 months. Turns out his pancreas was basically a raisin. Why the hell are doctors still treating symptoms like they're just 'stress'? We need mandatory blood panels for over-50s with unexplained weight loss. This isn't hype, it's negligence.
Frank Declemij
January 31, 2026 AT 16:02Early detection is the only real game-changer here. The data on new-onset diabetes as a biomarker is overwhelming-80% of patients develop it within 18 months prior to diagnosis. If primary care providers were trained to treat new diabetes in non-obese, non-diabetic adults as a red flag rather than a lifestyle issue, survival rates could improve dramatically. It's not complicated. It's just not prioritized.