NSAID Bleeding Risk Calculator
This tool estimates your risk of gastrointestinal bleeding from NSAID use based on factors from the article. Use this information to have a more informed conversation with your doctor.
Your Risk Assessment
This tool is for informational purposes only. Always consult your doctor before taking NSAIDs.
Every year, millions of people reach for ibuprofen, naproxen, or diclofenac to ease aching joints, headaches, or back pain. These are NSAIDs - non-steroidal anti-inflammatory drugs - and they work. But behind the relief is a quiet, often ignored danger: gastrointestinal bleeding. For many, especially older adults, what starts as a simple painkiller can lead to serious, even life-threatening complications. This isn’t a rare side effect. It’s common. And it’s preventable.
How NSAIDs Cause Damage
NSAIDs block enzymes called COX-1 and COX-2. COX-2 is involved in inflammation and pain, which is why these drugs help. But COX-1 protects the stomach lining by helping produce mucus and bicarbonate that shield the stomach from acid. When COX-1 is turned off, that protection disappears. The stomach lining gets exposed, erodes, and can develop ulcers. These aren’t always obvious. Some people feel nothing until they start vomiting blood, passing black tarry stools, or becoming weak from hidden, slow bleeding that leads to iron deficiency anemia.A 2020 meta-analysis in JAMA Internal Medicine found NSAID users are 3.2 to 4.2 times more likely to suffer upper gastrointestinal bleeding or perforation than non-users. That’s not a small risk. That’s a major one. And it doesn’t require a full-blown ulcer. Studies show that 86% of patients with NSAID-related lower GI bleeding never had a diagnosed peptic ulcer. The damage can happen anywhere - stomach, duodenum, even the small intestine.
Not All NSAIDs Are the Same
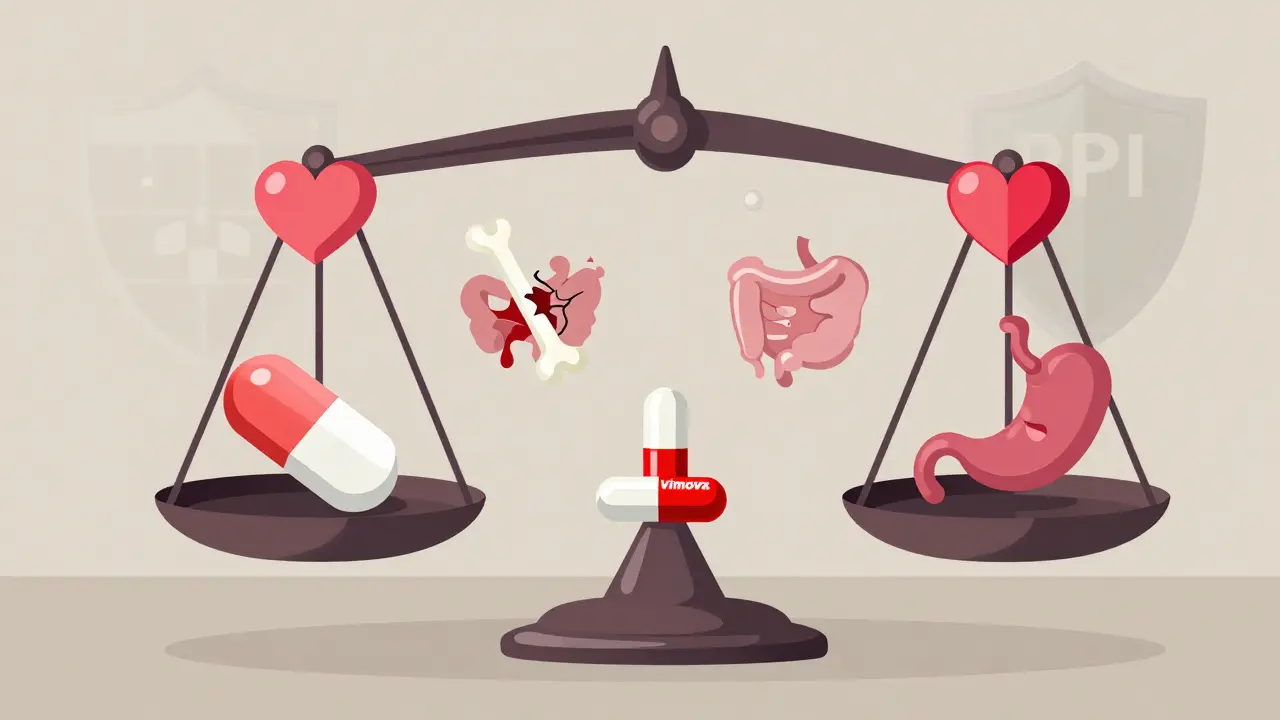
There’s a big difference between traditional NSAIDs and the newer COX-2 inhibitors. Drugs like ibuprofen, naproxen, and diclofenac block both COX-1 and COX-2. That means more stomach damage. Celecoxib and etoricoxib, on the other hand, mostly target COX-2. A 2000 Lancet study showed celecoxib had half the rate of serious ulcers compared to ibuprofen - 2.1 vs. 4.1 events per 100 patient-years.But here’s the trade-off: COX-2 inhibitors raise heart attack and stroke risk. The APPROVe trial in 2004 found rofecoxib (Vioxx) doubled the chance of heart attack. That’s why it was pulled from the market. Celecoxib still carries a warning, but it’s considered safer than older COX-2 drugs - if used at the lowest dose for the shortest time.
So if you need long-term pain relief and have risk factors, COX-2 inhibitors might be better for your stomach - but worse for your heart. The choice isn’t simple. It’s personal.
Who’s at Highest Risk?
Not everyone who takes NSAIDs bleeds. But some people are far more likely to. Experts have identified clear warning signs:- Age 70 or older - risk doubles every decade
- History of peptic ulcer or GI bleeding
- Taking blood thinners like warfarin or apixaban
- Using corticosteroids like prednisone
- Taking more than one NSAID at once
- Using high doses (over 1,200 mg/day of ibuprofen)
- Having serious conditions like heart failure, kidney disease, or liver cirrhosis
Dr. John D. Wolfe’s research showed that people with two or more of these factors have a 5x higher risk of bleeding. The American College of Gastroenterology uses a simple scoring tool: 2 points for age over 70, 2 for prior ulcer, 2 for anticoagulant use, and 1 for steroid use. A score of 2 or more means you’re high risk - and you need protection.
How to Protect Your Stomach
If you’re high risk, taking an NSAID without protection is like driving without a seatbelt. The good news? There are proven ways to cut the danger.Proton pump inhibitors (PPIs) - like omeprazole, esomeprazole, or pantoprazole - are the gold standard. A 2017 Cochrane review of over 13,000 patients found PPIs reduce NSAID-related ulcers by 75%. They’re effective, well-tolerated, and widely available. Many doctors now prescribe a PPI upfront for anyone over 65 taking NSAIDs regularly.
Misoprostol also reduces ulcers by 50-75%, but it causes diarrhea in up to 20% of users and abdominal pain in 15%. It’s not a first choice unless someone can’t take a PPI.
Then there’s Vimovo - a single pill combining naproxen and esomeprazole. Approved by the FDA in 2023, it’s designed for high-risk patients. In the PRECISION-2 trial, only 7.3% of people taking Vimovo developed ulcers, compared to 25.6% on naproxen alone. It’s not cheap, but for someone with a history of bleeding, it’s a game-changer.
What Patients Don’t Tell Their Doctors
Here’s the hidden problem: most people don’t report NSAID use - especially over-the-counter ones. A 2021 Clinics in Medicine review found 26% of users take more than the recommended dose. Many don’t realize OTC ibuprofen is still an NSAID. Others think, “It’s just a pill,” and never mention it during a check-up.On patient forums like HealthUnlocked, 63% of respondents had GI symptoms - nausea, bloating, dark stools - but only 37% told their doctor. On Reddit, users shared stories of elderly relatives ending up in the ER with severe anemia, needing blood transfusions, because no one connected the dots between daily ibuprofen and fatigue.
It’s not just about honesty. It’s about awareness. You can’t manage a risk you don’t know exists.
Real Numbers, Real Consequences
This isn’t theoretical. In the U.S. alone, NSAIDs cause about 107,000 hospitalizations and 16,500 deaths every year. The annual cost? Over $2.2 billion. Globally, the NSAID market is worth $11.3 billion - meaning millions are using them daily. The FDA has required black box warnings on all NSAIDs since 2005, clearly stating the risk of serious GI bleeding.And yet, people keep taking them. Why? Because they work. For arthritis, back pain, migraines - they’re often the most effective option. The goal isn’t to avoid them entirely. It’s to use them safely.
What Should You Do?
If you’re taking NSAIDs regularly, here’s what to ask yourself:- Am I using the lowest effective dose?
- Am I taking them for more than a few days at a time?
- Do I have any of the risk factors listed above?
- Have I told my doctor about every NSAID I take - even the ones bought over the counter?
- Am I on a PPI if I’m high risk?
If you’re over 65, have a history of ulcers, or take blood thinners - don’t wait for symptoms. Talk to your doctor about starting a PPI before continuing NSAIDs. If you’ve had bleeding before, COX-2 inhibitors with PPI are now the recommended approach. The American College of Rheumatology’s 2023 guidelines say: one risk factor? Use the lowest NSAID dose for the shortest time. Two or more? Use a COX-2 inhibitor with a PPI.
And if you’re feeling off - tired, pale, dizzy, or notice dark stools - get checked. Occult bleeding doesn’t scream. It whispers. And by the time it shouts, it’s too late.
What’s Next?
Scientists are working on safer options. New drugs called CINODs - COX-inhibiting nitric oxide donors - like naproxcinod, are in phase III trials. Early results show 50% fewer ulcers than naproxen, with less heart risk. They’re not on the market yet, but they’re promising.For now, the best strategy remains simple: know your risk, protect your stomach, and never assume an OTC pill is harmless. NSAIDs aren’t evil. But they’re powerful. And like any powerful tool, they need respect.
Can I take ibuprofen if I’ve had a stomach ulcer before?
If you’ve had a peptic ulcer or GI bleeding in the past, you should avoid traditional NSAIDs like ibuprofen unless absolutely necessary. The risk of another bleed is very high. Instead, talk to your doctor about using a COX-2 inhibitor like celecoxib along with a proton pump inhibitor (PPI). This combination offers the best protection for high-risk patients. Never restart NSAIDs without medical guidance after a bleeding episode.
Are over-the-counter NSAIDs safer than prescription ones?
No. OTC NSAIDs like ibuprofen and naproxen are the same drugs as prescription versions - just in lower doses. The risk of bleeding isn’t tied to whether the drug is prescribed or bought off the shelf. It’s tied to how much you take, how long, and your personal risk factors. Many people take OTC NSAIDs daily for years without telling their doctor, which makes it harder to spot danger signs. Always assume any NSAID - even one bought at the pharmacy - can cause serious stomach damage.
How do I know if I’m bleeding internally from NSAIDs?
Internal bleeding from NSAIDs can be silent. Signs include fatigue, dizziness, pale skin, shortness of breath, or dark, tarry stools (melena). Sometimes the only clue is unexplained iron deficiency anemia - low red blood cells from slow, ongoing blood loss. If you’re on long-term NSAIDs and feel unusually tired, ask your doctor for a blood test. A simple hemoglobin check can catch bleeding before it becomes an emergency.
Is it safe to take a PPI with NSAIDs long-term?
Yes, for high-risk patients, long-term PPI use with NSAIDs is not only safe - it’s recommended. PPIs like omeprazole are among the most studied drugs in medicine. While long-term use can slightly increase the risk of bone fractures or vitamin B12 deficiency, these risks are far lower than the risk of a life-threatening GI bleed. The American College of Gastroenterology supports continuous PPI therapy for patients with a history of ulcer bleeding who need ongoing NSAID treatment. Always use the lowest effective dose of PPI, and have your doctor review your need for it every 6-12 months.
What are alternatives to NSAIDs for chronic pain?
For chronic pain like arthritis, alternatives include acetaminophen (paracetamol), which has minimal GI risk but doesn’t reduce inflammation. Physical therapy, weight loss, heat/cold therapy, and topical pain relievers like diclofenac gel can help. In some cases, duloxetine or pregabalin may be prescribed for nerve-related pain. For severe cases, corticosteroid injections or even surgery may be options. Always discuss non-NSAID strategies with your doctor - especially if you’re at high risk for bleeding.
Payson Mattes
December 25, 2025 AT 11:08Okay but have you ever wondered if the NSA is secretly using NSAIDs to control the population? I mean, think about it - they’re everywhere, in every pharmacy, and they cause bleeding… just like how the government wants you docile and distracted. I read a classified memo once - no, seriously - that said COX-2 inhibitors were developed to mask symptoms so people wouldn’t notice how much their guts were rotting. They don’t want you healthy, they want you compliant. And PPIs? That’s just the next step - keeping you on meds forever so you never ask questions. I’ve got 17 spreadsheets on this. DM me if you want the sources.
Bhargav Patel
December 27, 2025 AT 07:17The pharmacological suppression of inflammation through COX inhibition presents a profound paradox: the alleviation of suffering is inextricably bound to the erosion of physiological integrity. One cannot but reflect upon the epistemic humility required to administer a substance that, while efficacious in its intended purpose, simultaneously dismantles the very mucosal defenses evolved over millennia to preserve homeostasis. The ethical weight of prescribing such agents - particularly in the absence of comprehensive risk stratification - demands not merely clinical acumen, but moral vigilance. We have, in our haste to relieve discomfort, outsourced the body’s wisdom to molecular intervention.
Steven Mayer
December 29, 2025 AT 05:03COX-1 inhibition leads to reduced prostaglandin E2 synthesis in gastric mucosa, which downregulates mucus and bicarbonate secretion, thereby increasing luminal H+ ion penetration and activating pepsinogen - a cascade that precipitates mucosal injury. The risk stratification models (like the ACG score) are statistically valid but clinically underutilized. PPIs reduce ulcer incidence via H+/K+ ATPase blockade, but long-term use alters gut microbiota composition, potentially increasing C. difficile susceptibility. The real issue? Most providers don’t screen for prior GI events or concomitant anticoagulant use before initiating NSAIDs. It’s not negligence - it’s systemic inertia.
Sidra Khan
December 30, 2025 AT 17:05So let me get this straight - you’re telling me ibuprofen is basically poison unless you’re also swallowing a $100 pill to undo the damage? 😂 I’ve been taking Advil for my period cramps since I was 16. My stomach’s fine. Also, I’m pretty sure my cat takes more NSAIDs than I do - she licks the counter after I drop one. 🐱💊
Ademola Madehin
December 30, 2025 AT 22:59Brooo this is wild 😭 I had my cousin in the ER last month - he was taking naproxen for his back pain every day for 3 years, never told anyone, then one day he just passed out in the bathroom. Blood everywhere. They had to transfuse 5 units. His mom cried for 2 days. I told him, "Man, you didn’t even know you were slowly bleeding out?" Now he’s on Vimovo and crying about the price. Life’s a joke, bro. 😭
suhani mathur
December 31, 2025 AT 20:46Oh sweetie, you really think the FDA’s black box warning is enough? 🙄 I’ve seen patients on 2400mg of ibuprofen daily for ten years, then blame "bad luck" when they show up with melena. The real tragedy isn’t the drug - it’s the cultural ignorance. People treat NSAIDs like aspirin candy. And yes, PPIs are the answer - but you don’t need to be a gastroenterologist to know that. Just ask your pharmacist. Or Google. Or, I don’t know, *talk to a doctor*. It’s not rocket science.
Diana Alime
January 1, 2026 AT 01:42i just took 2 ibuprofen for my headache and now i’m terrified. like… what if i’m bleeding internally?? i feel fine?? but what if i’m not?? i googled it and now i think i have 3 ulcers and my stomach is just… slowly dissolving?? 😭 i’m gonna go to the er. or maybe just drink milk. milk fixes everything. right??
Chris Buchanan
January 2, 2026 AT 04:53Let’s be real - this isn’t about fear. It’s about awareness. You don’t need to ditch NSAIDs. You just need to stop treating them like candy. If you’re over 60? Take a PPI. If you’re on blood thinners? Talk to your doctor. If you’ve had a bleed before? Don’t wing it. This isn’t complicated. You don’t need a PhD to read a warning label. Just be smart. Your gut will thank you. And if you’re still skeptical? Ask yourself: Would you drive without a seatbelt? No? Then don’t take NSAIDs without protection. Period.
Lindsey Kidd
January 4, 2026 AT 01:46❤️❤️❤️ This is the kind of post that saves lives. I’m a nurse and I’ve seen too many elderly patients come in with Hgb of 5 because they thought "it’s just a pill." Please, if you’re reading this - tell your grandma. Tell your dad. Tell your friend who takes ibuprofen like it’s a vitamin. Knowledge is power. And love. ❤️
Austin LeBlanc
January 5, 2026 AT 21:45Wow. Just wow. You wrote a 2000-word essay and still didn’t mention that NSAIDs are just a gateway drug to opioids. Everyone knows the pharmaceutical industry pushes these because they make you dependent. PPIs? That’s just the next product line. They want you on lifelong meds. You’re being played. Wake up.
niharika hardikar
January 7, 2026 AT 19:26The normalization of non-prescription NSAID consumption constitutes a profound failure of public health education. The conflation of analgesic accessibility with therapeutic innocuity reflects a broader epistemological decline in patient autonomy - wherein self-diagnosis supersedes clinical deliberation. The recommendation for PPI co-therapy is not merely prudent; it is ethically imperative for individuals possessing two or more risk factors. To neglect this is not negligence - it is a violation of the Hippocratic injunction to first, do no harm.