Medication-Induced Nosebleed Risk Checker
This tool helps you assess whether your medications might be contributing to frequent nosebleeds. Based on evidence from medical research, it evaluates your risk level and provides personalized prevention recommendations.
Important: This tool is for educational purposes only. It does not replace medical advice. Always consult your doctor before changing medications.
Risk Assessment
Getting a nosebleed isn’t rare - about 60% of people will have one at some point in their life. But when they start happening often, especially if you’re on regular medication, it’s not just annoying - it’s a signal. Many people don’t realize that common drugs they take for pain, allergies, or heart health can be the real reason behind those sudden, messy nosebleeds.
Why Medications Cause Nosebleeds
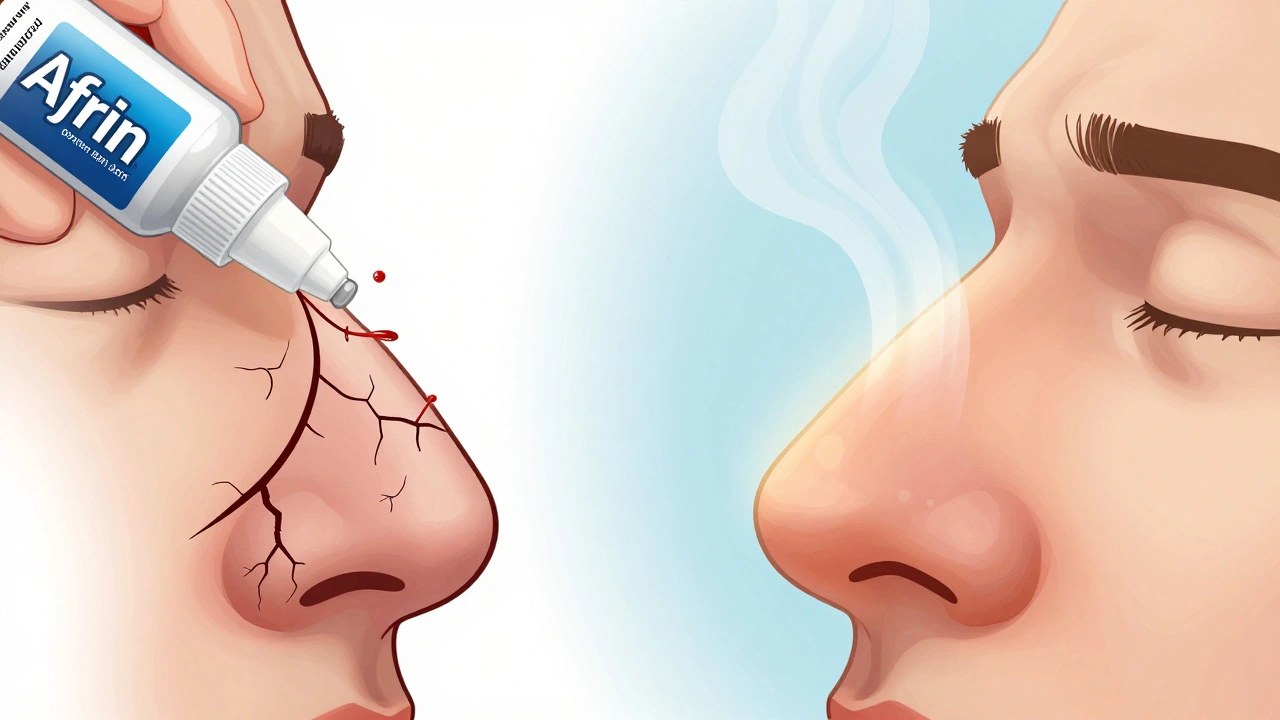
Nosebleeds happen because of the dense network of tiny blood vessels in the front of your nose, called Kiesselbach’s plexus. These vessels are close to the surface and easily damaged. Medications interfere in two main ways: by thinning your blood or by drying out your nasal lining. Drugs like aspirin, ibuprofen, and naproxen - all NSAIDs - block enzymes that help platelets stick together. That means even a small bump inside your nose can lead to bleeding that won’t stop quickly. It’s not just about taking too much. Even low-dose aspirin (81 mg daily), often taken to protect the heart, can do this. The same goes for prescription blood thinners like warfarin or clopidogrel. These don’t make your blood watery - they slow down the clotting process, so any tiny tear takes longer to seal. Then there are the decongestants. Sprays like oxymetazoline (Afrin) give quick relief for a stuffy nose, but using them for more than three days in a row backfires. They shrink blood vessels at first, then cause rebound swelling and dryness. Your nasal lining gets thin, cracked, and more likely to bleed. Antihistamines for allergies do the same thing - they reduce mucus but leave your nose feeling parched.Which Medications Are Most Likely to Cause Nosebleeds?
Some medications are far more linked to nosebleeds than others. Here’s what the evidence shows:- Aspirin - Even low-dose versions used for heart protection can increase bleeding risk.
- NSAIDs - Ibuprofen (Advil, Motrin), naproxen (Aleve), and ketoprofen all interfere with platelet function.
- Warfarin (Coumadin) - A classic blood thinner that affects vitamin K-dependent clotting factors. If your INR level is too high, nosebleeds become more frequent and harder to stop.
- Clopidogrel (Plavix) - An antiplatelet drug often prescribed after stents or strokes. It doesn’t affect INR, but still increases bleeding time.
- Decongestant nasal sprays - Oxymetazoline and phenylephrine sprays cause rebound congestion and mucosal damage if used longer than 3 days.
- Antihistamines - Oral ones like loratadine or cetirizine dry out nasal passages over time.
- Heparin - Can trigger a rare but serious reaction called heparin-induced thrombocytopenia (HIT), which can cause unusual bleeding, including nosebleeds, about a week after starting.
It’s not just about the drug - it’s about how you’re using it. Taking multiple NSAIDs at once, or combining them with aspirin, multiplies the risk. Older adults, especially those on several medications, are at higher risk simply because their nasal tissue is naturally thinner and drier.
Who’s Most at Risk?
Some groups are more likely to have medication-related nosebleeds:- Adults over 45 - Nasal membranes thin with age. Add medication use, and the risk climbs.
- Children - They pick their noses more often, and even mild medications can tip the balance.
- Pregnant women - Hormones cause blood vessels in the nose to expand. Combine that with prenatal vitamins containing iron (which can dry out the nose) or pain relievers, and nosebleeds become common.
- People with high blood pressure or atherosclerosis - Higher pressure in the vessels makes them more likely to rupture.
- People on multiple medications - Drug interactions can amplify side effects. For example, taking warfarin and ibuprofen together is a known red flag.
If you’re on any of these meds and notice your nosebleeds are more frequent - say, three or four times a week - it’s not normal. It’s time to look at your medication list.
How to Prevent Medication-Induced Nosebleeds
Prevention is simpler than you think - and it doesn’t mean stopping your meds without talking to your doctor.- Switch to acetaminophen - For pain or fever, use Tylenol instead of ibuprofen or aspirin. It doesn’t affect platelets or clotting.
- Moisturize daily - Apply a thin layer of petroleum jelly (Vaseline) inside each nostril twice a day, especially before bed. Saline nasal gels work too.
- Use a humidifier - Especially in winter, when indoor air drops below 30% humidity. A cool-mist humidifier near your bed helps keep nasal passages moist.
- Avoid nose picking or blowing hard - This is the #1 trigger. If you need to clear your nose, do it gently. Use saline spray first.
- Limit decongestant sprays - Never use nasal sprays longer than 3 days in a row. If congestion returns, talk to your doctor about alternatives like steroid sprays.
- Stay hydrated - Drink enough water. Dehydration makes your mucus thicker and your nasal lining more fragile.
These steps don’t just reduce nosebleeds - they help your nasal tissue heal. Many people see a big drop in frequency within a week of starting these habits.
What to Do When a Nosebleed Happens
If you get a nosebleed, don’t panic. And definitely don’t tilt your head back - that sends blood down your throat, which can make you gag or even vomit. Follow these steps:- Lean slightly forward - this lets the blood drain out your nose.
- Pinch the soft part of your nose shut - just below the bony bridge - with your thumb and index finger.
- Hold for 10 to 15 minutes. Use a timer. Most people give up too soon.
- Breathe through your mouth.
- After 15 minutes, release slowly. Don’t blow your nose for the next few hours.
If it doesn’t stop after 20 minutes, or if you feel dizzy, lightheaded, or notice bruising elsewhere, go to urgent care. For people on blood thinners, even a short nosebleed can be serious - call your doctor immediately.

When to Talk to Your Doctor
Don’t ignore recurring nosebleeds - especially if you’re on medication. Your doctor might not realize it’s linked until you bring it up. Schedule a review if you have:- More than three or four nosebleeds in a week
- Nosebleeds that last longer than 20 minutes
- Bleeding that starts after starting a new medication
- Other signs of easy bruising or bleeding (gums, cuts, urine)
Your doctor may check your INR if you’re on warfarin, or suggest switching medications. Sometimes, a pharmacist can help spot risky combinations you didn’t know about. Never stop a blood thinner or heart medication on your own - the risk of a clot or stroke is far greater than the risk of a nosebleed.
Final Thoughts
Nosebleeds from medications are preventable - but only if you connect the dots. It’s not always the drug itself, but how it interacts with your body, your environment, and your habits. Simple changes like moisturizing your nose, avoiding nasal sprays beyond three days, and choosing acetaminophen over ibuprofen can cut nosebleeds in half.If you’ve been living with frequent nosebleeds and assuming it’s just “dry air” or “allergies,” think again. Your meds might be the missing piece. Talk to your doctor, review your list, and take back control - your nose will thank you.

Paul Dixon
December 10, 2025 AT 12:59I used to get nosebleeds every other week until I switched from ibuprofen to Tylenol. No joke, within a week they stopped. I thought it was just dry winter air, turns out my meds were the real culprit.
Now I slap Vaseline in my nose before bed like it’s lotion. Weird? Maybe. Effective? Absolutely.
Monica Evan
December 11, 2025 AT 19:46OMG YES this is the most real thing ive read all week
my mom was on warfarin and kept bleeding out her nose like a horror movie
doc said 'its just aging' but i knew better
we cut out the NSAIDs and started saline spray and holy cow it stopped
why do doctors never mention this stuff till you're drowning in blood
ps i use coconut oil now instead of vaseline its cheaper and smells like vacation
Taylor Dressler
December 11, 2025 AT 23:39It’s important to clarify that while NSAIDs increase bleeding risk by inhibiting platelet aggregation, they do not affect the coagulation cascade directly like anticoagulants (e.g., warfarin or heparin). This distinction matters clinically because the mechanisms differ, and so do the reversal strategies.
Additionally, the recommendation to use acetaminophen as a substitute is sound, but patients with liver disease should be cautioned. Always consider the full pharmacological profile before switching.
Moisturizing the nasal mucosa with saline gel or petrolatum is one of the most underutilized preventive measures in primary care - and it’s backed by solid evidence.
Aidan Stacey
December 13, 2025 AT 07:20MY NOSE HAS BEEN SOBBING FOR YEARS AND NO ONE TOLD ME IT WAS THE MEDS??
I thought I was just a walking tragedy with a bloody face every morning
Now I’m crying because I didn’t know this sooner
It’s not dry air. It’s not allergies. It’s not fate.
It’s a damn pill I’ve been swallowing like a good little zombie.
Thank you for this. I’m going to hug my humidifier tonight.
Jean Claude de La Ronde
December 14, 2025 AT 17:39So let me get this straight - we live in a society where you can buy a gun easier than you can get a doctor to admit that your 81mg aspirin is turning your nasal passages into a dripping faucet?
Also, Vaseline? Really? That’s our modern medical breakthrough?
Next they’ll tell us to rub butter on our arteries to fix heart disease.
Also, I’m pretty sure my nosebleeds are caused by capitalism. But sure, let’s blame the aspirin.
Lisa Stringfellow
December 16, 2025 AT 07:41Wow. Another ‘you’re probably just doing it wrong’ article.
So I’m supposed to stop my blood thinner because I get nosebleeds? What if I have a stroke tomorrow? Oh wait, that’s not your problem, right?
And who even uses Vaseline anymore? That’s what my grandma used in the 70s.
Also, I’ve tried all this. It didn’t work. So obviously it’s my fault. I’m just too weak to handle my own body.
Aman deep
December 17, 2025 AT 10:52Bro i live in delhi and my nose bleeds every monsoon
thought it was pollution but then i realized my blood pressure med was the problem
switched to losartan and started using aloe vera gel inside nose
no more blood on my pillow
also humidifier is a game changer
india needs more of this kind of info in local languages
thank u for writing this
Eddie Bennett
December 18, 2025 AT 16:40Been on Plavix since my stent. Got nosebleeds every few weeks. Tried everything - humidifier, saline, you name it.
Then one day I just stopped using Afrin. Like, cold turkey. Didn’t even taper.
Three days later - zero bleeds.
Turns out the spray was wrecking my nasal lining more than the meds.
So yeah, sometimes the fix isn’t the drug you’re on - it’s the drug you’re using on top of it.
Sylvia Frenzel
December 19, 2025 AT 08:46People in America are so weak. In my country, we just deal with nosebleeds. We don’t run to the doctor, we don’t buy humidifiers, we don’t switch meds.
We just bleed. And we’re stronger for it.
Also, Vaseline? That’s a product of Big Pharma marketing.
Real men use a tissue and a prayer.
Doris Lee
December 20, 2025 AT 16:55This made me feel so seen
I’ve been getting nosebleeds since I started prenatal vitamins
Never thought it was the iron drying me out
Now I’m using a tiny bit of coconut oil before bed and it’s like my nose finally got a hug
You’re a lifesaver
Also - don’t let anyone tell you this isn’t a real thing
It’s real. And it sucks. And you’re not alone
Michaux Hyatt
December 22, 2025 AT 13:44One thing I always tell my patients: if you’re on multiple medications, get a med review with your pharmacist.
They’re the unsung heroes of drug safety.
They catch interactions doctors miss because they’re rushing between appointments.
And yes - combining warfarin with ibuprofen is basically playing Russian roulette with your nasal blood vessels.
Don’t be shy - ask them. They love it.
Raj Rsvpraj
December 24, 2025 AT 01:15Oh, so now we’re blaming aspirin? How quaint. In my country, we have real science - not this pseudo-medical folk wisdom. Did you know that the Kiesselbach plexus is not even the primary source of epistaxis in 40% of cases? You’re oversimplifying. Also, Vaseline? That’s a petroleum byproduct. You’re poisoning yourself. Use aloe vera, you fool. And stop using ‘saline spray’ - it’s just salt water. You’re paying $12 for tap water. Pathetic.
Jack Appleby
December 24, 2025 AT 19:29Let me correct some misconceptions here. While NSAIDs inhibit COX-1 and reduce platelet aggregation, the effect is reversible and transient - unlike clopidogrel, which irreversibly binds P2Y12 receptors. Also, the claim that low-dose aspirin increases nosebleed risk is only significant in meta-analyses with high heterogeneity. The absolute risk increase is less than 0.5% per year. And Vaseline? Please. The real solution is intranasal topical tranexamic acid - it’s FDA-approved for this indication. But no, let’s just smear petroleum jelly and call it a day. Typical American overcorrection.
Frank Nouwens
December 25, 2025 AT 20:51While the information presented is generally accurate and well-intentioned, it is essential to emphasize that any alteration of pharmacotherapy must be conducted under the supervision of a qualified healthcare provider. The cessation or substitution of anticoagulant or antiplatelet agents without clinical guidance may result in catastrophic thromboembolic events. The preventive measures outlined - including humidification and nasal moisturization - are adjunctive and should not be considered substitutes for professional medical evaluation. Further, the use of petroleum-based products in the nasal cavity carries a theoretical risk of lipid pneumonia, though exceedingly rare in clinical practice.