Medication Brain Fog Risk Calculator
This tool helps you identify medications that might be causing brain fog and memory issues. Based on the Anticholinergic Cognitive Burden (ACB) scale, it calculates your risk level and suggests safer alternatives.
Medications You're Taking
Add each medication you're currently taking to assess your brain fog risk
Results
How to Use This Tool
1. Add all medications you're currently taking
2. Click "Calculate Risk Score"
3. Review your risk level and high-risk medications
4. Discuss results with your healthcare provider
Note: This is not a medical diagnosis. Always consult your doctor before making any medication changes.
Ever had one of those days where you walk into a room and forget why? Or stare at your phone, unable to remember your own password? If you’re taking any medications regularly, it might not be just stress or aging - it could be your pills.
Brain fog and memory lapses from medications are more common than most people realize. And the scary part? These symptoms are often reversible. Unlike Alzheimer’s or other neurodegenerative diseases, when the culprit drug is identified and adjusted, mental clarity can return - sometimes within days.
What Medications Cause Brain Fog?
Not all drugs affect your brain the same way. Some hit your memory centers hard, while others barely register. The biggest offenders fall into a few key categories.
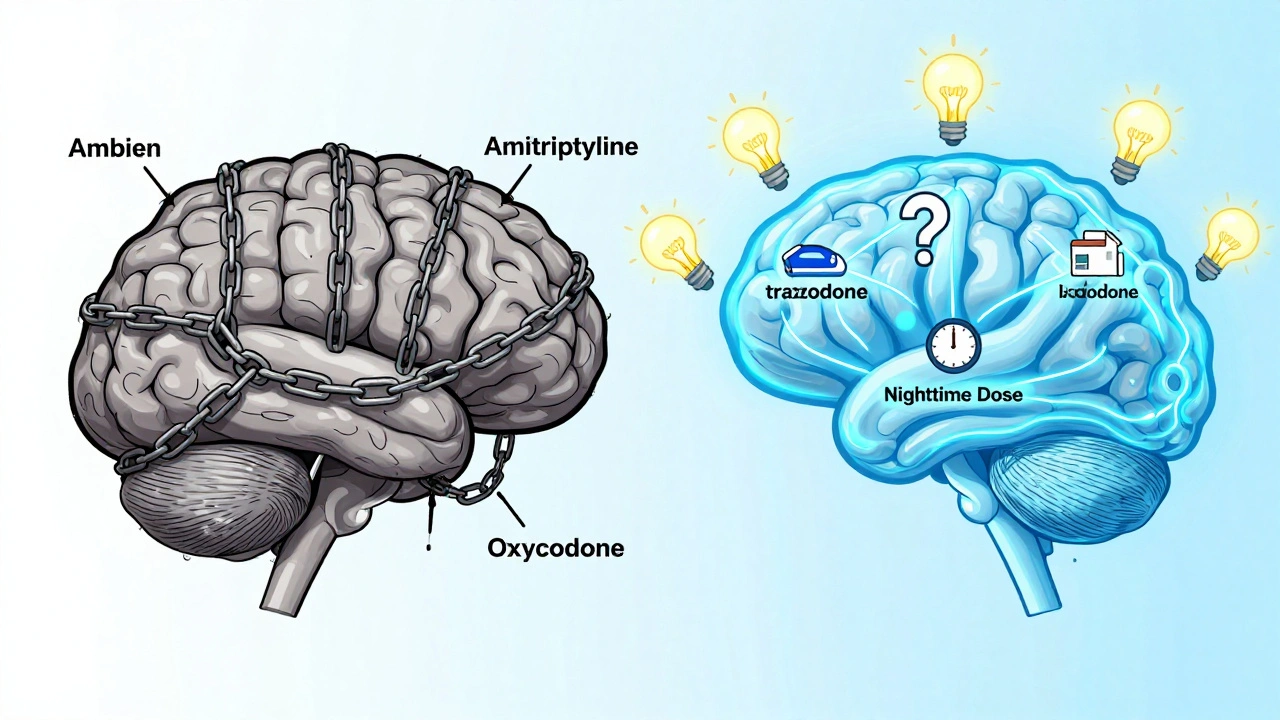
Anticholinergic drugs are the top cause. These block acetylcholine, a chemical your brain needs to form memories and stay alert. Common examples include diphenhydramine (Benadryl, Tylenol PM), oxybutynin (Ditropan for overactive bladder), and tricyclic antidepressants like amitriptyline. A 2011 NIH study found people taking these had a 4.2 times higher risk of memory problems than those who didn’t. Regular use of diphenhydramine over seven years increases dementia risk by 54%, according to a JAMA Internal Medicine study.
Benzodiazepines like alprazolam (Xanax) and hypnotics like zolpidem (Ambien) slow down activity in the hippocampus and prefrontal cortex - the areas responsible for turning short-term memories into long-term ones. Studies show they can reduce memory transfer by up to 30%. Ambien users report memory gaps in 15% of cases, compared to just 5% with lorazepam.
Opioids - oxycodone, hydrocodone, codeine - bind to receptors in the medial temporal lobe and blunt working memory. At standard doses, users experience a 25% drop in their ability to hold and process information. Immediate-release versions cause even more disruption than long-acting ones.
Chemotherapy doesn’t just attack cancer cells. About 75% of patients develop what’s called “chemo brain,” with trouble focusing, remembering names, or following conversations. For 35% of them, these issues last months or years after treatment ends.
Even statins - the cholesterol-lowering pills - have been blamed, though the evidence is mixed. A 2013 JAMA study of over 1,000 people found no real difference in memory between statin users and placebo groups. But individual cases are real: some people swear their brain fog cleared the moment they stopped taking them.
Why Does This Happen?
Your brain runs on a delicate balance of chemicals. Neurotransmitters like acetylcholine, serotonin, and GABA are the messengers that keep your thoughts flowing. Medications disrupt this system - not because they’re “bad,” but because they’re powerful.
Anticholinergics don’t just dry your mouth - they block signals your brain uses to recall where you put your keys. Benzodiazepines don’t just make you sleepy - they dampen the brain’s ability to consolidate memories during sleep. Opioids don’t just numb pain - they quiet the parts of your brain that handle attention and working memory.
And it’s not just the drug itself. Age, liver function, genetics, and other medications all play a role. Someone over 65 metabolizes drugs slower. Someone with a CYP2D6 gene variant might process a drug much faster or slower than average. Two people on the same dose of the same pill can have completely different experiences.
Who’s Most at Risk?
Older adults are the most vulnerable. About 30% of seniors experience noticeable cognitive side effects from medications. But it’s not just age. People taking five or more prescriptions are at much higher risk. That’s because drug interactions multiply the effect.
Consider this real scenario: A 70-year-old woman takes diphenhydramine for allergies, amitriptyline for nerve pain, and zolpidem for sleep. Each one is anticholinergic or sedating. Together, they create a perfect storm for brain fog. Her doctor might not realize it - until she starts forgetting her grandkids’ names.
Even younger people aren’t safe. A Reddit user reported complete memory blackouts after two weeks of 5mg Ambien. The symptoms vanished within 72 hours of stopping it. That’s not rare. Over 140 similar stories exist on that thread alone.

How to Tell If It’s Your Medication - Not Aging
Brain fog from drugs has a signature pattern:
- Symptoms start shortly after beginning or increasing a dose - often within days or weeks.
- You notice it most in the morning, after taking nighttime meds.
- You feel mentally “sluggish,” not confused or disoriented like in dementia.
- Your memory gaps are about recent events - not long-term recall.
- When you stop the drug, your thinking clears up.
Compare that to Alzheimer’s: memory loss is progressive, affects long-term memories, and doesn’t reverse. If your confusion came on fast and improved after skipping a pill, it’s likely medication-related.
One telltale sign: if you’ve been taking an OTC sleep aid like Benadryl for years and now feel foggy all day, it’s probably the culprit. These drugs aren’t meant for long-term use - yet millions take them nightly.
What to Do If You Suspect Your Medication Is the Cause
Don’t quit cold turkey. But do take action.
- Make a list of every pill, supplement, and OTC product you take. Include dosages and times. Don’t forget herbal teas, sleep aids, or cough syrup.
- Look for red flags. Check if any contain diphenhydramine, doxylamine, or are labeled “anticholinergic.”
- Ask your doctor about the Anticholinergic Cognitive Burden (ACB) scale. Many hospitals now use this tool to rate drugs by their brain impact. A score of 3 means high risk.
- Request a medication review. Ask: “Could any of these be causing my brain fog?”
- Try one change at a time. If you’re on three suspect drugs, don’t drop them all. Work with your doctor to pause one for two weeks, then reassess. If your brain clears up, you’ve found your trigger.
For sleep aids, switching to melatonin (0.5-5mg) or trazodone (25-50mg) often helps. Studies show 85% of people regain mental clarity within two weeks.
For pain, consider duloxetine (Cymbalta) instead of opioids. It’s just as effective for nerve pain but causes 40% less cognitive disruption.
And if you’re taking an antihistamine for allergies, switch from diphenhydramine to loratadine (Claritin) or cetirizine (Zyrtec). They’re just as effective for sneezing - but 3-5 times less likely to fog your brain.
Timing Matters
Even if you can’t switch a drug right away, timing can help. Taking sedating meds at night - not in the morning - cuts daytime brain fog by 35%, according to a Johns Hopkins study. If you’re on a medication that makes you drowsy, take it right before bed. That simple change can make a noticeable difference.
What’s Changing in Medicine?
Doctors are waking up to this problem. The Beers Criteria - the gold standard for safe prescribing in older adults - now lists 52 high-risk medications. Hospitals using these guidelines have cut medication-related cognitive issues by 28%.
The FDA now requires stronger warnings on benzodiazepines about memory loss. Electronic health records now flag high anticholinergic burden automatically.
New drugs are coming. Daridorexant, a next-gen sleep aid in Phase III trials, shows 92% less cognitive impact than Ambien. And pharmacogenomic testing - checking your genes to see how you metabolize drugs - is becoming more common. One 2024 trial showed a 63% drop in brain fog when prescriptions were tailored to a patient’s DNA.
Medicare now pays pharmacists to review medications for cognitive risk. By 2026, 15 million beneficiaries will get this service.
Final Thoughts
Brain fog from medication isn’t a sign of failing memory - it’s a sign your body is reacting to something you’re taking. The good news? You have more control than you think.
You don’t need to suffer through cloudy thinking because “it’s just aging.” You don’t need to accept memory lapses as normal if you’re on a sleep aid or painkiller. These are side effects - and they’re often reversible.
Start with your list. Talk to your doctor. Make one change. Give it two weeks. You might be surprised how clear your mind becomes.
Can over-the-counter sleep aids cause brain fog?
Yes - especially those containing diphenhydramine or doxylamine, like Benadryl, Tylenol PM, or Unisom. These are strong anticholinergics that block acetylcholine, a key brain chemical for memory. Regular use over years increases dementia risk by 54%. Switching to melatonin or trazodone often clears brain fog within days to weeks.
How long does it take for brain fog to go away after stopping a medication?
It varies. For most people, symptoms begin improving within 3-7 days after stopping a drug like Ambien or diphenhydramine. Full recovery can take up to 14 days. For drugs that build up in the system - like tricyclic antidepressants - it may take 3-6 weeks. Patience is key, but improvement is almost always seen if the medication was the cause.
Are antidepressants linked to memory problems?
Some are. Tricyclic antidepressants like amitriptyline have strong anticholinergic effects and are linked to a 4.2-fold higher risk of memory issues. SSRIs like sertraline or escitalopram have much lower risk - only about 1.8 times higher than non-users. If you’re on an older antidepressant and experiencing brain fog, ask your doctor if switching to an SSRI could help.
Can statins cause memory loss?
The evidence is mixed. Large studies show no significant difference in memory between statin users and placebo groups. But individual cases are real - some people report mental clarity returning after stopping. If you suspect statins are affecting you, don’t stop them without talking to your doctor. Instead, ask about non-statin alternatives like ezetimibe or PCSK9 inhibitors, which don’t cross the blood-brain barrier.
Is brain fog from medication permanent?
No - it’s usually temporary. Unlike Alzheimer’s or other neurodegenerative diseases, medication-induced cognitive impairment reverses when the drug is stopped or switched. Studies show cognitive function improves by 15-20% on standard tests within 4-6 weeks of removing high-risk medications. The brain is resilient. Give it time and the right adjustments.
What should I ask my doctor about my medications?
Ask: “Could any of these be causing my brain fog?” Request a review of your list using the Anticholinergic Cognitive Burden (ACB) scale. Ask if any drugs can be switched to lower-risk alternatives - like loratadine instead of diphenhydramine, or trazodone instead of Ambien. And ask about timing: could taking a sedating pill at night instead of morning help?”

Shofner Lehto
December 4, 2025 AT 12:31My grandma was on Benadryl for years and started forgetting where she put her glasses, then her keys, then her own birthday. Took her off it and within two weeks she was back to telling stories from the 60s like it was yesterday. Doctors need to stop treating old people like they’re just supposed to be foggy.
Yasmine Hajar
December 5, 2025 AT 02:19THIS. I was on Ambien for six months and thought I was losing my mind. Couldn’t remember conversations, forgot my dog’s name for three days. Stopped cold turkey (bad idea, but I was desperate) and my brain came back like a rebooted laptop. If you’re on sleep meds and feel like you’re walking through syrup - get off them. Your brain isn’t broken, your pharmacy is.
Karl Barrett
December 6, 2025 AT 11:57The neuropharmacological mechanism underlying anticholinergic-induced cognitive impairment is well-documented in the literature - particularly the downregulation of muscarinic M1 receptors in the hippocampal circuitry, which directly impairs synaptic plasticity and long-term potentiation. What’s concerning is the normalization of this effect in clinical practice. The ACB scale isn’t just a tool - it’s a diagnostic imperative. Yet most primary care providers still prescribe diphenhydramine like it’s aspirin. We’re not just overlooking side effects - we’re institutionalizing iatrogenic cognitive decline.
Jake Deeds
December 6, 2025 AT 21:59Wow. So now we’re blaming pills for not being able to remember where you left your phone? I mean, I get it - you’re all so busy scrolling through TikTok and forgetting your own name that you need a scapegoat. But maybe it’s not the meds. Maybe it’s your brain. Or your life. Or the fact that you’ve been medicating your existence with caffeine, sugar, and Netflix since 2012. Just saying.
val kendra
December 7, 2025 AT 07:28Stop taking Benadryl. Seriously. Just stop. Try melatonin 1mg. Or just go to bed earlier. Your body doesn’t need a chemical nap. I switched from amitriptyline to sertraline and my fog lifted in 10 days. No drama. No panic. Just a better choice. Your brain is not a toaster. Don’t keep putting the wrong thing in it.
Isabelle Bujold
December 7, 2025 AT 14:23I’ve been researching this for over a year now and I’ve come to realize that the pharmaceutical industry has been quietly weaponizing sedation as a treatment modality for decades. The fact that statins are even approved for long-term use without mandatory cognitive screening is a moral failure. And don’t get me started on how benzodiazepines are still prescribed for anxiety like they’re candy - they’re not, they’re neurotoxic, slow-release memory erasers. The FDA’s warnings are too little too late. What we need is a complete overhaul of psychiatric prescribing culture, not just a list of ‘high-risk’ drugs. We’re treating symptoms instead of systems, and people are paying the price with their mental clarity.
Chad Handy
December 8, 2025 AT 04:26I’ve been on 7 different meds for 11 years. I don’t remember my wife’s birthday, I don’t remember why I walked into the kitchen, I don’t remember if I even have a wife anymore. My doctor says ‘it’s just aging.’ I say it’s the cocktail of drugs they’ve been dumping into me like it’s a science experiment. I’m not 80, I’m 48. I used to be able to recite Shakespeare. Now I can’t remember my own damn name. And no one cares. They just write another script.
Augusta Barlow
December 9, 2025 AT 16:20They don’t want you to know this, but the FDA and Big Pharma have been suppressing data on cognitive side effects since the 90s. The 54% dementia risk from Benadryl? That study got buried. The Johns Hopkins study on timing? Never mentioned in ads. Why? Because if people realized how many of their meds are brain-damaging, they’d stop buying them. And that would cost billions. This isn’t medicine. It’s corporate control disguised as care. Your fog? It’s not accidental. It’s engineered.
Joe Lam
December 10, 2025 AT 05:01Wow. So now we’re all just supposed to be cognitive experts and self-diagnose drug side effects? Next you’ll be telling me I should check my own liver enzymes before taking ibuprofen. This is why people think they know more than their doctors. You’re not a pharmacologist. You’re not even a nurse. Stop Googling and let the professionals do their job. Or at least stop scaring people with half-baked Reddit science.
Jenny Rogers
December 10, 2025 AT 12:13It is both lamentable and profoundly concerning that the medical establishment has permitted the widespread and unregulated administration of anticholinergic agents to geriatric populations without implementing mandatory cognitive baseline assessments. The ethical ramifications of such negligence are not merely clinical - they are existential. One must ask: in an age of precision medicine, why do we still permit the blunt instrument of polypharmacy to be wielded with such cavalier disregard for neurocognitive integrity? The answer, I fear, lies not in ignorance, but in institutional inertia - a systemic failure of moral imagination.
Rachel Bonaparte
December 11, 2025 AT 14:42Let me guess - you’re one of those people who thinks ‘natural remedies’ are the answer. Melatonin? Please. That’s just a fancy sleep placebo. And switching to Zyrtec? Oh sure, because allergies are just in your head. You think this is about pills? No. It’s about control. They want you dependent. They want you docile. They want you too foggy to ask why your blood pressure med makes you forget your kid’s name. Wake up. This isn’t medicine. It’s mind control with a prescription label.
Scott van Haastrecht
December 13, 2025 AT 04:05Every single one of you is missing the point. This isn’t about drugs. It’s about the fact that we’ve turned our brains into disposable hardware. We don’t sleep right. We don’t eat right. We don’t move. We’re addicted to screens and sugar and stress. Then we take a pill to fix the symptoms of our own self-inflicted chaos. And now we’re surprised we feel like zombies? You’re not being poisoned by meds - you’re being poisoned by your lifestyle. And you’re too lazy to change it. So you blame the pill. Pathetic.
Chase Brittingham
December 14, 2025 AT 14:45I’m not a doctor but I’ve been on 6 meds for chronic pain and anxiety. I felt like my thoughts were underwater. Took me 3 months to get off one thing at a time with my doctor’s help. My brain didn’t come back overnight - but after 6 weeks, I remembered what it felt like to read a book and actually understand it. I cried. Not because I was sad. Because I was finally clear. If you’re reading this and you feel foggy - don’t give up. Talk to someone. One change. One week. You might be surprised.