Most people don’t realize that the pill in their bottle could cost 90% less - and it’s not because they’re getting a cheaper brand. It’s because of generic drugs and authorized generics. If you’re paying full price for a prescription, you’re likely leaving hundreds - even thousands - of dollars on the table every year. The good news? You don’t need a degree in pharmacology to get these savings. You just need to know what to ask.
What’s the Difference Between Generic and Authorized Generic Drugs?
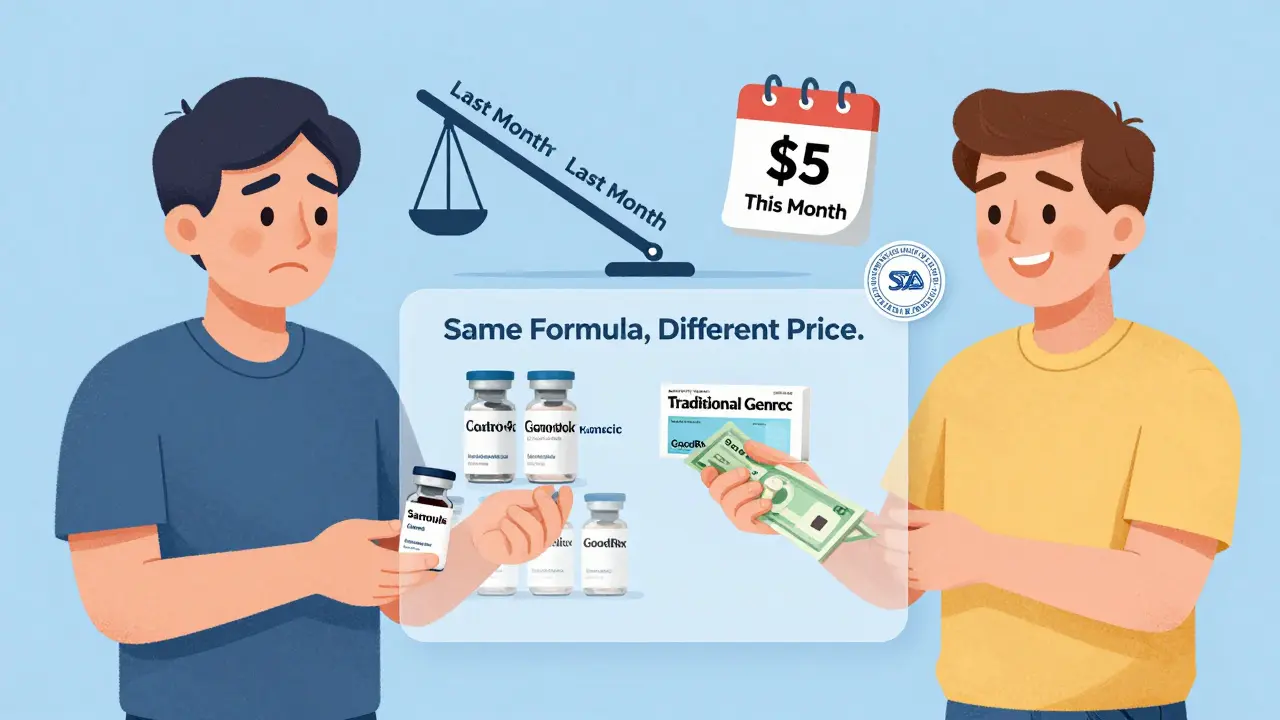
Generic drugs are copies of brand-name medications that become available after the original patent expires. They have the same active ingredients, strength, dosage, and effect as the brand version. The FDA requires them to be bioequivalent - meaning they work the same way in your body. That’s not marketing. That’s science. Authorized generics are different. They’re made by the same company that produces the brand-name drug, but sold under a generic label. Think of it like a car manufacturer making the exact same model but selling it under a different nameplate. You get the same factory, same formula, same packaging - just a lower price tag. Here’s the catch: even though they’re identical, insurance plans often treat them differently. One might be on a lower copay tier than the other. That’s why asking the right questions matters more than just picking the first generic you see.Why Generics Save You So Much Money
In 2022, generic drugs saved the U.S. healthcare system over $408 billion. That’s not a typo. Over $400 billion in one year. And most of that savings should be flowing to you. When a brand-name drug loses its patent, prices drop fast. Within a year, the cost can fall by more than 75%. Some drugs - like the HIV medication Truvada - went from $50 per pill down to $3. That’s a 94% drop. The first generic usually causes the biggest price plunge. Each additional generic competitor pushes prices down another 10-15%. But here’s where it gets tricky. The list price you see on a drug’s sticker isn’t always what you pay. Insurance companies, pharmacy benefit managers (PBMs), and rebate deals shuffle money behind the scenes. A generic might have a $10 list price, but your copay is $25 because your plan doesn’t cover it well. That’s why asking about how your insurance treats generics is just as important as asking if one exists.How to Ask Your Pharmacist the Right Questions
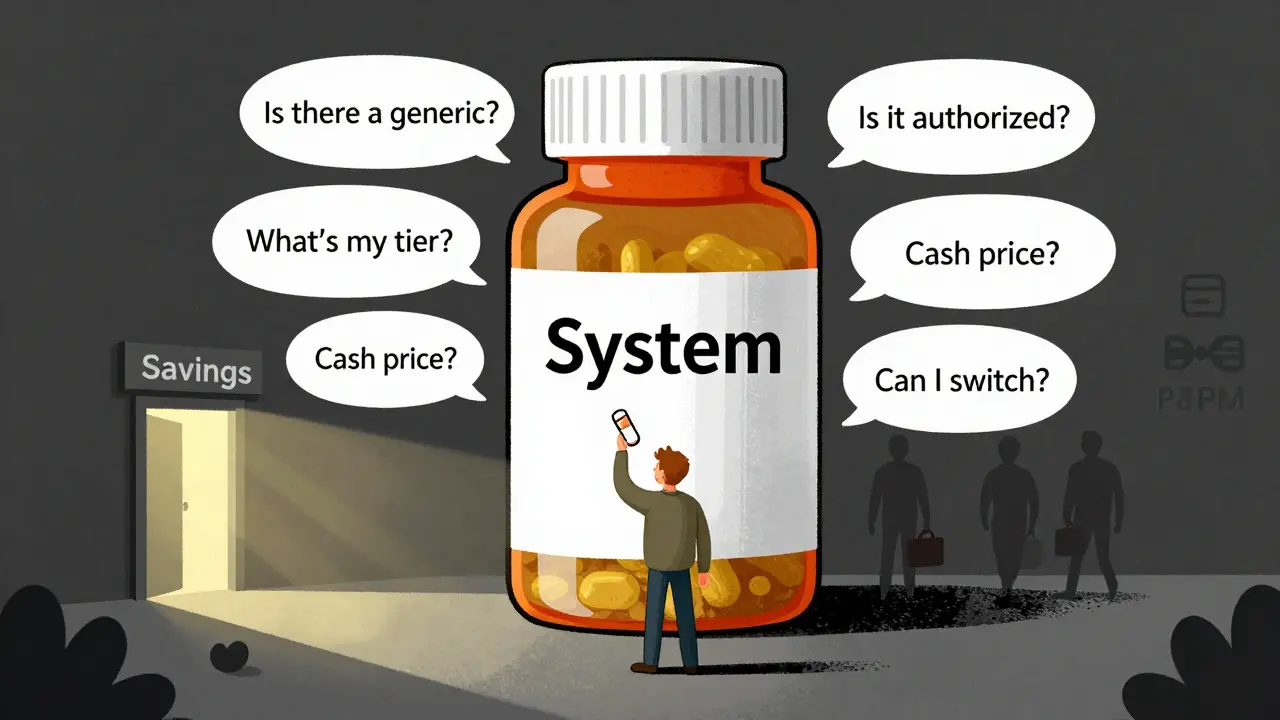
Most pharmacists know generics exist. But only 43% of independent pharmacists can clearly explain the difference between an authorized generic and a traditional generic when it comes to your out-of-pocket cost. So you need to lead the conversation. Here’s exactly what to say:- “Is there a generic version of this medication?”
- “Is this an authorized generic?”
- “How does my insurance handle authorized generics versus regular generics?”
- “Can I switch between them to save money?”
- “What’s the cash price if I don’t use insurance?”
Authorized Generics: More Savings - or a Trap?
Authorized generics often have lower wholesale prices than brand-name drugs. In some cases, they’re priced 50-67% lower. But because they’re made by the brand company, they sometimes aren’t subject to the same rebate negotiations that traditional generics go through. That means your insurer might not pass along the savings. In some cases, brand manufacturers use authorized generics to delay competition. They release their own generic version right when the patent expires, so no other company can jump in for 180 days. That’s legal - but it keeps prices higher than they’d be if multiple generics flooded the market. The good news? This tactic is becoming less common. The FDA and FTC are cracking down on practices that delay generic entry. But until that changes, you need to be smart.Use Tools to Compare Prices
Your pharmacist isn’t always the best source for real-time pricing. That’s where apps like GoodRx, SingleCare, and RxSaver come in. They show you cash prices at nearby pharmacies - for both traditional and authorized generics. One patient in Texas found that the authorized generic version of his blood pressure pill cost $12 cash at Walgreens, but the traditional generic was $4 at CVS. He switched - and saved $8 every month. That’s $96 a year. For a medication he takes every day. These apps also show you when a drug is on a special discount. Sometimes, the cash price is lower than your insurance copay. That’s not rare. It’s common.What About Your Insurance Plan?
Your plan’s formulary - the list of drugs it covers - determines your out-of-pocket cost more than the drug itself. Two identical pills can have different copays because one is on Tier 1 and the other on Tier 2. Call your insurance provider. Ask:- “What tier is this generic on?”
- “Is the authorized generic covered differently than the traditional generic?”
- “Can I get a prior authorization to switch to a cheaper generic?”
Why Some People Still Pay Too Much
Even though 93% of generic prescriptions cost under $20, 28% of patients still pay more than $20 per month for a generic. Why? - High-deductible plans make you pay full price until you hit your deductible.- PBMs don’t always pass savings to consumers.
- Some insurers treat authorized generics as “brand” drugs for pricing purposes.
- Pharmacists don’t always know the difference - and don’t offer alternatives. The solution? Be proactive. Don’t wait for your refill. Every time you get a new prescription, ask the five questions above. Even if you’ve been on the same drug for years - new generics appear all the time.
What You Can Do Today
You don’t need to wait for your next doctor’s visit. Here’s your action plan:- Check your current prescription. Is it brand-name? If yes, ask your pharmacist: “Is there a generic?”
- If there is, ask: “Is it an authorized generic?”
- Use GoodRx to compare cash prices for both types.
- Call your insurance and ask about formulary tiers.
- Switch if you find a better option - even if it’s the same medicine.
Final Thought: You’re Not Paying for the Pill - You’re Paying for the System
The medication itself is cheap. The system around it isn’t. But you have more power than you think. You’re not just a patient. You’re a consumer. And you deserve to pay what the drug actually costs - not what the system charges. Start asking. Start comparing. Start saving.Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they work the same way in your body. Generics are held to the same manufacturing standards. Over 90% of prescriptions in the U.S. are generics - and they’ve been safely used for decades.
What’s the difference between an authorized generic and a regular generic?
An authorized generic is made by the same company that produces the brand-name drug, often in the same factory, but sold under a generic label. A regular generic is made by a different company after the brand’s patent expires. Both are FDA-approved and therapeutically identical. The key difference is pricing and how insurance treats them - authorized generics sometimes have higher copays because they’re not subject to the same rebate deals.
Why is my copay the same for a brand and a generic?
Your insurance plan might not have updated its formulary, or it could be treating the generic as a brand-name drug - especially if it’s an authorized generic. Some plans put authorized generics on higher tiers because they’re made by the brand company. Always check your plan’s formulary or call your insurer to confirm the tier for each version.
Can I save money by paying cash instead of using insurance?
Yes, often. Many generic drugs cost less out-of-pocket than your insurance copay. For example, a 30-day supply of a generic blood pressure pill might be $4 at CVS with GoodRx, but your copay could be $15. Always compare cash prices using apps like GoodRx before using insurance - especially for generics.
How often should I check if a cheaper generic is available?
Check every time you refill - or at least every 6 months. New generics appear constantly. A drug that had no generic last year might have two today. The FDA approves hundreds of new generics each year. Don’t assume your current option is still the cheapest.
Do authorized generics delay cheaper generics from entering the market?
Yes, sometimes. Brand manufacturers can release an authorized generic right after patent expiration, blocking other companies from entering for up to 180 days. This delays competition and keeps prices higher than they’d be with multiple generics. While this practice is declining, it still happens - especially with high-cost drugs like insulin and biologics.
Are there any drugs that don’t have generics?
Yes. Some drugs - especially complex ones like inhalers, injectables, and certain skin creams - are hard to copy. Others are still under patent. But over 90% of prescriptions in the U.S. are for drugs that have generic versions. If yours doesn’t have one yet, ask your doctor if there’s a similar drug that does.

Bryan Woods
December 26, 2025 AT 14:53Interesting breakdown. I never realized authorized generics could be priced higher than regular ones due to insurance tiering. I’ve been using GoodRx for years, but I always assumed any generic was automatically cheaper. Learned something today.
Ryan Cheng
December 28, 2025 AT 02:31Y’all need to stop treating your pharmacist like a vending machine. They’re not just handing out pills-they’re trained to help you save money. Ask the five questions. Do it every time. Even if you’ve been on the same med for five years. New generics drop all the time. I saved $180 last year just by asking ‘Is this authorized?’
wendy parrales fong
December 28, 2025 AT 20:47It’s wild how something so simple-asking a question-can change your whole financial life. I used to just take what the pharmacy gave me. Then I started asking. Now I save over $200 a year on my thyroid med. It’s not magic. It’s just paying attention. We all deserve to not be ripped off just because we’re sick.
Jeanette Jeffrey
December 30, 2025 AT 04:02Oh wow, another ‘ask your pharmacist’ post. Real revolutionary. Meanwhile, the system is rigged. PBMs, brand manufacturers, insurance loopholes-it’s all a pyramid scheme disguised as healthcare. You think asking nicely fixes that? LOL. You’re just feeding the machine. Go live in Canada.
Shreyash Gupta
December 31, 2025 AT 01:58Bro I tried this. Asked for generic. Got authorized. Saved $5. Then I checked GoodRx. Cash price was $1. I cried. Then I cried harder because I paid $30 last month. 😭💸
Ellie Stretshberry
December 31, 2025 AT 14:09i never knew authorized generics were different from regular ones... i just thought generic = cheap... i just switched my blood pressure med last month and saved like 40 bucks a month... i feel kinda dumb for not asking sooner lol
Zina Constantin
January 2, 2026 AT 00:55As someone who grew up in a country where medicine is subsidized, I never realized how broken the U.S. system is. You’re not just paying for the pill-you’re paying for bureaucracy, greed, and confusion. This post is a lifeline. Share it with your parents. Share it with your friends. This is healthcare justice.
Dan Alatepe
January 2, 2026 AT 12:36Man... I just lost my job last month. My insulin was $500. I found the generic on GoodRx for $12. I almost hugged the pharmacist. Then I cried. Then I posted this on my mom’s Facebook group. She’s 68. She didn’t even know generics existed. We’re all just trying to survive.
Angela Spagnolo
January 3, 2026 AT 16:05...I just realized... I’ve been paying $25 for my antidepressant for three years... and the cash price is $7... I didn’t even know... I’m so embarrassed... I’m calling my insurance right now... I’m so overwhelmed... I didn’t know I could do this... I feel like a fool...
Sarah Holmes
January 4, 2026 AT 11:06While I appreciate the sentiment, this post is dangerously naive. The system is not broken-it is functioning exactly as designed. Corporations profit from your ignorance. Asking questions is performative activism. It does not change the structural exploitation of patients by pharmaceutical monopolies, PBMs, and insurance cartels. You are being manipulated into believing you have agency when you do not.
Jay Ara
January 4, 2026 AT 11:46bro this is gold i used to think generic meant bad quality now i know its just the brand playing games i switched my cholesterol med and saved 60 a month no more stress
Michael Bond
January 5, 2026 AT 23:15Ask the five questions. Do it now.
Kuldipsinh Rathod
January 6, 2026 AT 23:29My uncle in Mumbai pays $1 for his blood pressure pills. Here I paid $22. Same drug. Same factory. Just different labels. This isn’t healthcare. It’s a global scam.