If you have multiple sclerosis (MS), you know how unpredictable the symptoms can be. One of the most common but often overlooked issues is nerve pain-sharp, burning, or electric-like sensations that don’t respond to regular painkillers. That’s where gabapentin comes in. It’s not a cure for MS, but for many people, it’s one of the few things that actually helps with the pain that makes daily life feel impossible.
What is gabapentin?
Gabapentin is an anticonvulsant medication originally developed to treat seizures. But over time, doctors noticed it worked well for another kind of pain: nerve pain. It doesn’t work like aspirin or ibuprofen. Instead, it calms down overactive nerves that send wrong signals to the brain. In MS, damaged nerves misfire, causing pain even when there’s no injury. Gabapentin helps reduce those false alarms.
The brand name Neurontin is still common, but most people now take generic gabapentin. It comes in capsules, tablets, and oral solutions. Doses usually start low-300 mg once a day-and slowly increase over weeks. Many people end up taking 900-3,600 mg daily, split into three doses. It’s not instant. It can take two to four weeks before you notice real relief.
Why do MS patients take gabapentin?
Multiple sclerosis attacks the protective coating around nerves, called myelin. When that coating breaks down, nerves send chaotic signals. This leads to several types of pain:
- Neuropathic pain: Burning, tingling, or stabbing sensations in limbs, face, or torso
- Spasticity-related pain: Muscle stiffness and cramps that feel like constant tightening
- Lhermitte’s sign: A sudden electric shock feeling down the spine when bending the neck
A 2021 study in the Journal of Neurology, Neurosurgery & Psychiatry tracked 127 MS patients using gabapentin for nerve pain. Over half reported at least a 30% reduction in pain scores after eight weeks. That’s not just a little better-it’s enough to get out of bed, walk to the kitchen, or sleep through the night.
It’s not just about pain. Some people with MS use gabapentin to help with sleep disruption caused by nerve discomfort. Others find it reduces muscle spasms enough to make physical therapy more tolerable.
How does gabapentin compare to other MS pain treatments?
There are other options, but each has trade-offs:
| Treatment | How it works | Common side effects | Speed of relief | Best for |
|---|---|---|---|---|
| Gabapentin | Calms overactive nerves | Drowsiness, dizziness, swelling | 2-4 weeks | Generalized nerve pain, burning sensations |
| Pregabalin (Lyrica) | Similar to gabapentin, but stronger | Weight gain, blurred vision, dizziness | 1-2 weeks | Severe pain, faster need |
| Tricyclic antidepressants (e.g., amitriptyline) | Alters brain chemicals that process pain | Dry mouth, constipation, drowsiness | 3-6 weeks | Pain + depression or sleep issues |
| Cannabinoids (e.g., Sativex) | Targets cannabinoid receptors in nerves | Dizziness, dry mouth, fatigue | 1-2 weeks | Spasticity + pain, where legal |
| NSAIDs (e.g., ibuprofen) | Reduces inflammation | Stomach upset, kidney strain | Hours | Muscle soreness, not nerve pain |
Gabapentin is often the first choice because it’s affordable, widely available, and doesn’t interact badly with most MS disease-modifying therapies. Pregabalin works faster and sometimes stronger, but it’s more expensive and causes more weight gain. Antidepressants help if you’re also struggling with mood, but they’re not ideal if you’re already feeling tired. Cannabinoids are promising but restricted in many places, including parts of the UK.
What are the side effects of gabapentin?
Most people tolerate gabapentin okay, but side effects are common-especially at first. The most frequent ones:
- Drowsiness (up to 40% of users)
- Dizziness or unsteadiness (especially in older adults)
- Swelling in hands or feet
- Blurred vision
- Feeling “foggy” or mentally slow
These usually fade after a few weeks as your body adjusts. But if dizziness makes you fall, or if you feel unusually tired, talk to your doctor. Never stop gabapentin suddenly-it can cause seizures or severe withdrawal. Tapering off takes weeks.
Some people report mood changes, including anxiety or depression. If you notice new or worsening sadness, irritability, or thoughts of self-harm, contact your healthcare provider immediately. This is rare, but serious.
Who shouldn’t take gabapentin for MS?
Gabapentin isn’t for everyone. Avoid it if you:
- Have kidney problems (it’s cleared by the kidneys-dose must be lowered)
- Are pregnant or breastfeeding (limited safety data)
- Have a history of drug misuse (it can be misused, though less than opioids)
- Are already taking strong sedatives or opioids (risk of dangerous breathing suppression)
If you’re over 65, your doctor will start you on a lower dose. Older adults are more sensitive to dizziness and falls.
What does real-life use look like?
Emma, 48, was diagnosed with relapsing-remitting MS five years ago. Her hands and feet burned constantly, especially at night. She tried ibuprofen, heat pads, even acupuncture. Nothing worked. Her neurologist suggested gabapentin.
“I started at 100 mg at bedtime. First week, I felt like a zombie. Second week, the dizziness got better. By week three, I slept through the night for the first time in months. Now I take 300 mg three times a day. The burning hasn’t vanished, but it’s down to a dull ache. I can hold my coffee cup without wincing. That’s life-changing.”
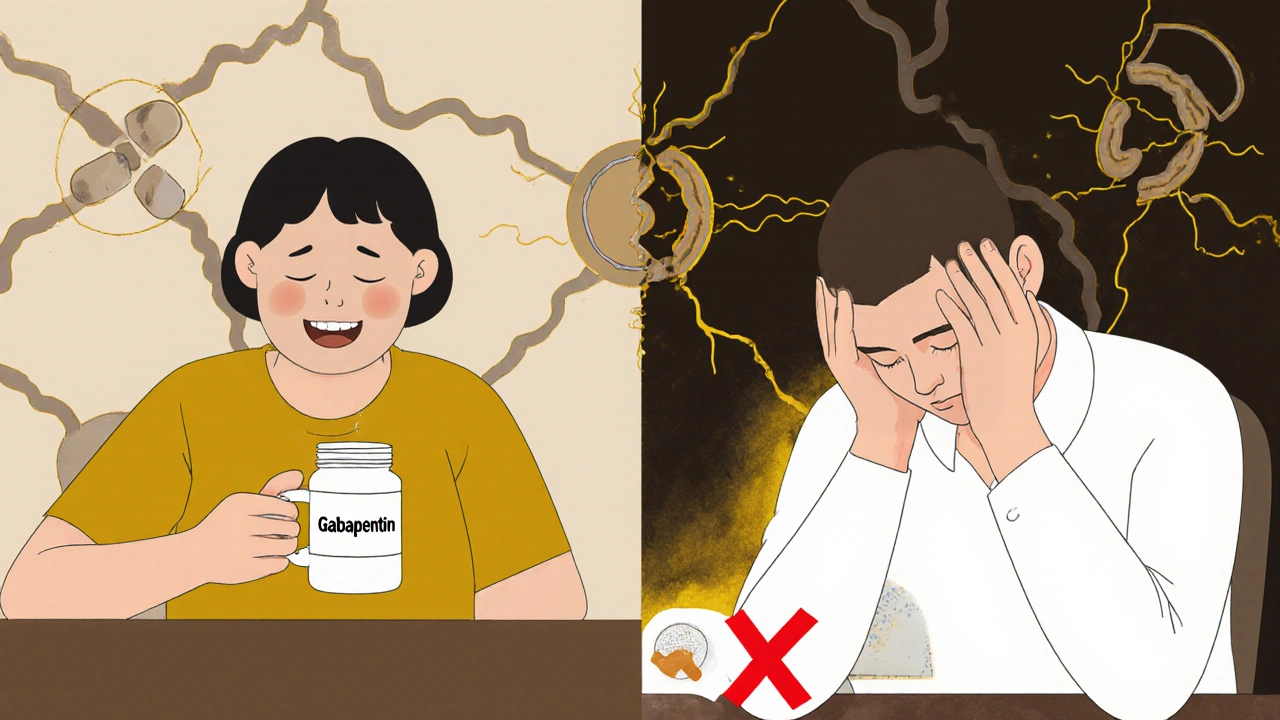
Not everyone has that result. James, 57, tried gabapentin for three months. “It made me too drowsy to work. I couldn’t focus on my computer. I stopped it.”
That’s the reality: gabapentin helps some people enormously, helps others a little, and doesn’t help some at all. It’s not a magic pill. But it’s one of the most reliable tools we have for MS nerve pain.

How to get the most out of gabapentin
If your doctor prescribes it, here’s how to make it work:
- Start low and go slow. Don’t rush the dose increase. Your body needs time to adjust.
- Take it with food if it upsets your stomach.
- Keep a pain diary. Note when the pain is worst, what you’re doing, and how you feel after taking the dose. This helps your doctor fine-tune your plan.
- Don’t drink alcohol. It makes drowsiness and dizziness worse.
- Don’t drive or operate heavy machinery until you know how it affects you.
- Be patient. Give it at least six weeks before deciding it’s not working.
Some people find combining gabapentin with gentle exercise-like tai chi or water aerobics-makes the pain more manageable. Others benefit from cognitive behavioral therapy (CBT) to cope with chronic pain. Gabapentin doesn’t fix the root cause of MS, but it can give you back control over your daily life.
Frequently Asked Questions
Can gabapentin slow down MS progression?
No. Gabapentin only treats symptoms like nerve pain and muscle spasms. It does not affect the underlying immune attack on the nervous system. Disease-modifying therapies like interferons, ocrelizumab, or fingolimod are used to slow MS progression. Gabapentin is a symptom manager, not a disease modifier.
Is gabapentin addictive?
It’s not addictive in the way opioids are, but some people develop dependence. That means your body gets used to it, and stopping suddenly can cause withdrawal symptoms like anxiety, insomnia, nausea, or even seizures. Always taper off under medical supervision. Misuse is rare, but possible-especially in people with a history of substance use disorders.
How long do I need to take gabapentin for MS pain?
There’s no set time limit. Many people take it long-term if it works and side effects are manageable. MS symptoms can change over time, so your doctor will check in every few months. If your pain improves or new treatments become available, you might reduce or stop it. But don’t stop on your own-even if you feel fine.
Can I take gabapentin with my other MS medications?
Yes, in most cases. Gabapentin doesn’t interfere with common MS drugs like interferons, dimethyl fumarate, or natalizumab. But always tell your neurologist about everything you’re taking-including supplements and over-the-counter meds. Some drugs, like antacids, can reduce gabapentin absorption. Take them at least two hours apart.
What if gabapentin doesn’t work for me?
You’re not alone. About 30-40% of people don’t get enough relief from gabapentin alone. Your doctor might try pregabalin, amitriptyline, or a low-dose antidepressant. Non-drug options like physical therapy, TENS units, or mindfulness training can also help. Sometimes combining two approaches gives better results than one alone. Don’t give up-there are other tools.
Next steps
If you’re considering gabapentin for MS pain:
- Track your symptoms for a week-when they happen, how bad they are, what makes them better or worse.
- Write down your questions before your next appointment. Bring your pain diary.
- Ask your neurologist: “Is gabapentin right for my type of pain?” and “What’s the plan if it doesn’t work?”
- Don’t buy gabapentin online or from friends. It’s a prescription drug for a reason-dosing matters.
Living with MS is hard. But managing pain doesn’t have to be a guessing game. Gabapentin isn’t perfect, but for many, it’s the quiet hero that lets them get back to living-not just surviving.

Jenny Lee
November 18, 2025 AT 20:56Gabapentin saved my nights. No more screaming from burning feet. I can finally sleep. Game changer.
Jeff Hakojarvi
November 19, 2025 AT 12:41Been on gabapentin for 3 years with MS. Started at 100mg, now at 2700mg split three ways. Side effects faded after month. Drowsiness? Yeah. But I’d rather be sleepy than in pain. Pro tip: take it with food. Less stomach drama. And never quit cold turkey-my doc made me taper over 6 weeks. Felt like withdrawal from a bad ex, but way less emotional.
Jonathan Gabriel
November 20, 2025 AT 23:34So… we’re just accepting that our nervous system is a glitchy wifi router and gabapentin is the reboot button? Interesting. No one’s asking why the damn router keeps breaking. MS isn’t just nerve pain-it’s an immune system throwing a tantrum. Gabapentin’s just putting a bandaid on a nuclear leak. But hey, if it lets you hold a coffee cup without crying… I guess I’ll take it. Still feels like we’re treating symptoms like they’re the disease. And why’s it cheaper than my artisanal kombucha?
Don Angel
November 21, 2025 AT 05:52Just wanted to say… thank you for writing this. So clear. So helpful. I’ve been scared to ask my neurologist about gabapentin because I didn’t want to sound like I was self-diagnosing. But now I feel ready. I’m printing this out. And I’m taking it with food. And not driving until I know how it hits me. And… yeah. I’m keeping a pain diary. Thank you.
benedict nwokedi
November 22, 2025 AT 09:50Let me guess… Big Pharma pushed this because it’s patent-expired and they’re milking it like a cash cow. Gabapentin? It’s just a cheap sedative disguised as medicine. Meanwhile, real solutions-like vitamin D megadoses or cannabis oil-are being suppressed. You think this is science? It’s corporate control. And don’t get me started on how they’re hiding the link between glyphosate and MS. Gabapentin’s just another pill to keep you docile while they poison the water supply.
kim pu
November 22, 2025 AT 17:29Gabapentin? More like Gabapain. I took it for two weeks and felt like my brain was wrapped in wet socks. My neuro said ‘it’s just adjusting’-yeah, adjusting to being a zombie. I swapped it for CBD oil and now I can actually think. Also, why are we still using 90s meds when we got terpenes and quantum biofeedback? Just saying. #MSHack
Kevin Jones
November 23, 2025 AT 04:16There’s a metaphysical layer here. Pain isn’t just biological-it’s existential. Gabapentin doesn’t fix the broken myelin, but it lets you sit with the silence that follows. That silence? That’s where healing begins. Not in the pill. In the pause. In the breath after the electric shock fades. We treat symptoms like enemies. But what if they’re just messengers? Gabapentin doesn’t silence the message-it lets you hear it without screaming.
Saket Sharma
November 24, 2025 AT 20:28Typical American medical laziness. Gabapentin? Easy fix. No real rehab. No diet overhaul. No detox. You think a pill solves MS? You’re delusional. In India, we use yoga, turmeric, and fasting. Real medicine. Not this chemical crutch. You’re just trading pain for brain fog. Pathetic.
Shravan Jain
November 25, 2025 AT 11:07While the article presents a superficially comprehensive overview of gabapentin's pharmacological profile in the context of multiple sclerosis, it conspicuously omits any critical analysis of the placebo effect magnitude in neuropathic pain trials, the confounding influence of concurrent psychotropic medication usage, or the longitudinal neuroadaptive changes induced by chronic GABAergic modulation. Furthermore, the anecdotal testimonials lack methodological rigor and introduce significant selection bias. One must question the epistemological validity of such evidence-based narratives when they are uncritically disseminated in public forums.
Brandon Lowi
November 25, 2025 AT 16:46Why is the FDA letting Big Pharma push this foreign-made junk on American patients? Gabapentin’s made in China, you know. And they’re pumping it into our veterans, our seniors, our kids. This isn’t medicine-it’s a slow invasion. We need real American pain relief. Not some overseas chemical that makes you zone out like a zombie. Wake up, people. This is cultural surrender.
Richard Couron
November 25, 2025 AT 17:57They’re drugging us to keep us quiet. Gabapentin? It’s not for pain. It’s for compliance. You think your neurologist cares if you can sleep? No. They care that you’re not screaming in the ER. They care that you’re not posting videos online about how the system failed you. They want you docile. Calm. Quiet. Gabapentin doesn’t fix your nerves-it fixes your mouth. And don’t even get me started on how they’re hiding the link to autism in kids born to moms on it. Google it. I dare you.
Alex Boozan
November 26, 2025 AT 15:19The real issue isn’t gabapentin-it’s the systemic failure of neurology to invest in regenerative therapies. We’re using band-aids while the lab has stem cells that could rebuild myelin. But why fund cures when you can sell a $2 generic pill for 20 years? This isn’t medicine. It’s capitalism with a stethoscope. And we’re all just patients in a profit model.
mithun mohanta
November 26, 2025 AT 15:58Oh wow, gabapentin. The holy grail of neurologists who don’t want to do real work. You know what’s better? Ketogenic diet. I went keto for 6 months, cut out gluten, and my burning sensation vanished. Gabapentin? That’s just a chemical crutch for people who don’t want to change their lifestyle. Also, I read a paper-actually, I skimmed a headline-that said gut microbiome dysbiosis is the real root. So… maybe stop taking pills and start eating sauerkraut? Just a thought.
Ram tech
November 27, 2025 AT 20:30This article is overly optimistic. Most patients report minimal benefit. The 30% reduction statistic is cherry-picked. In clinical practice, over half of MS patients discontinue gabapentin due to side effects or inefficacy. The author ignores the high dropout rate and the fact that pregabalin, while more expensive, often yields superior outcomes. This is not evidence-based-it’s promotional.