Natural Remedy Recommendation Tool for Proctitis
Find Your Best Remedy
Answer these questions to get personalized recommendations based on your symptoms and preferences.
Your Recommended Remedy
Quick Takeaways
- Proctitis is inflammation of the rectal lining that often causes pain, bleeding, and urgency.
- Diet, hygiene, and lifestyle tweaks can lessen symptoms, but they rarely replace medical therapy.
- Eight well‑studied natural options-Aloe vera, coconut oil, apple cider vinegar, probiotic yogurt, chamomile tea, sitz baths, psyllium husk, and turmeric-have varying evidence levels.
- Use a single remedy at a time, start with low doses, and stop if irritation worsens.
- Seek medical help if bleeding persists, you develop fever, or symptoms last more than two weeks.
What Is Proctitis?
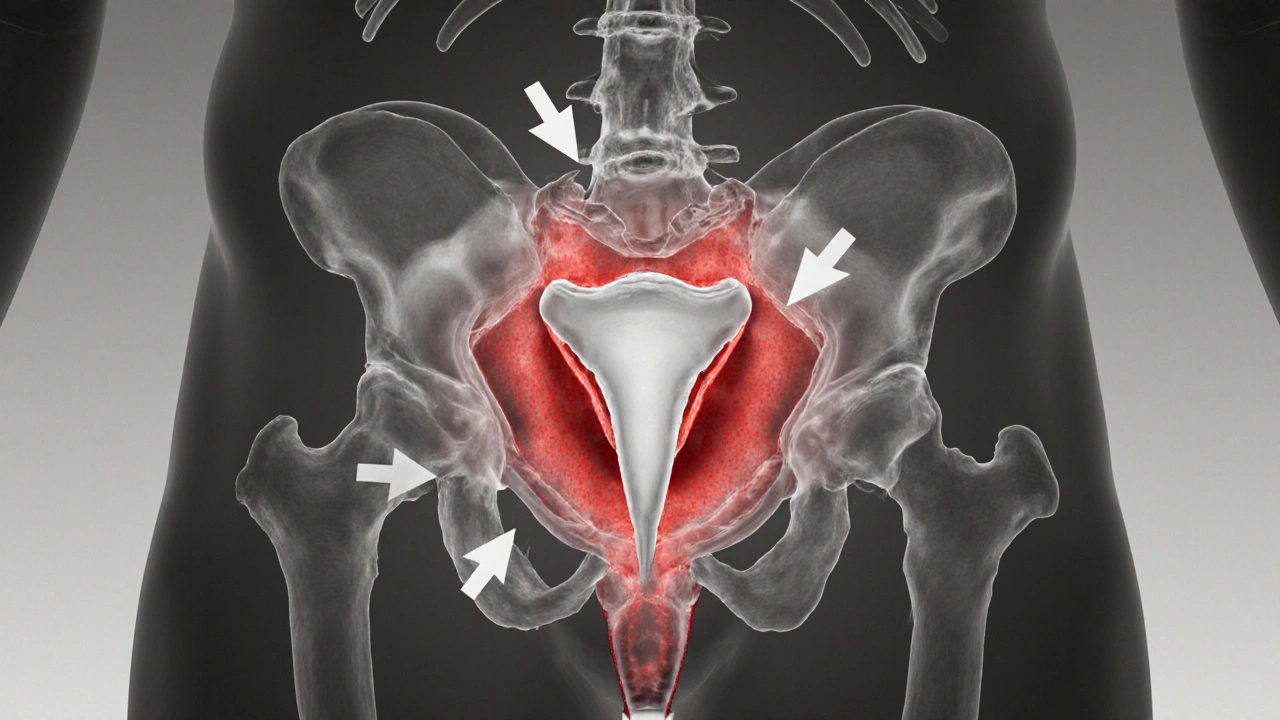
Proctitis is inflammation of the lining of the rectum, the final section of the large intestine. It can result from infections, inflammatory bowel disease, radiation therapy, or an overgrowth of harmful bacteria. Typical signs include abdominal cramping, urgency to defecate, blood‑stained mucus, and a burning sensation during bowel movements.
Because the rectum is close to the skin, irritation often spreads to the perianal area, making hygiene a crucial part of management. While doctors usually prescribe topical steroids or antibiotics, many patients look for gentler, at‑home options to complement prescription drugs.
Why Consider Natural Remedies?
Natural remedies appeal for three main reasons: they are generally affordable, they have a lower risk of systemic side effects, and they can be incorporated into daily routines without a prescription. However, "natural" does not automatically mean "safe"-some plants or oils can irritate the delicate rectal mucosa if used incorrectly.
Understanding the science behind each remedy helps you pick the ones that actually soothe inflammation rather than just mask pain.
Top Natural Options and How They Work
-
Aloe vera gel contains anthraquinones and aloins that exhibit anti‑inflammatory and antimicrobial properties. Applied as a thin layer after a sitz bath, it can reduce redness and promote healing.
-
Coconut oil is rich in lauric acid, a fatty acid with proven antibacterial activity. A warm, sterile spoonful applied topically can create a protective barrier, keeping the area moist and reducing friction during bowel movements.
-
Apple cider vinegar (unfiltered, with the "mother") supplies acetic acid, which can help balance the local pH and deter pathogenic bacteria. Dilute one tablespoon in a cup of warm water and use it as a sitz bath solution.
-
Probiotic yogurt supplies live cultures of Lactobacillus and Bifidobacterium. Regular consumption (about 150ml daily) can restore a healthy gut microbiome, indirectly reducing rectal inflammation.
-
Chamomile tea contains bisabolol and chamazulene, compounds shown to calm mucosal irritation. A warm chamomile sitz bath for ten minutes can ease pain without chemicals.
-
Sitz bath (a shallow warm water soak) itself is a cornerstone of symptom relief. Warm water at 38-40°C improves blood flow, softens stool, and flushes irritants.
-
Psyllium husk is a soluble fiber that bulks stool and reduces straining. One teaspoon mixed with water, taken twice daily, can smooth bowel movements and limit mechanical trauma to inflamed tissue.
-
Turmeric (curcumin) has robust anti‑inflammatory effects demonstrated in multiple gut studies. A daily capsule delivering 500mg of standardized curcumin, taken with black pepper for better absorption, may lower systemic inflammation that aggravates proctitis.

Quick Comparison of Common Remedies
| Remedy | Active Component | Typical Use | Evidence Level | Safety Notes |
|---|---|---|---|---|
| Aloe vera | Aloin, anthraquinones | Topical gel after sitz bath | Small RCTs (moderate) | Patch test first; avoid if allergic |
| Coconut oil | Lauric acid | Warm topical layer 2-3times/day | Observational (low) | May feel greasy; rare irritation |
| Apple cider vinegar | Acetic acid | 1Tbsp in 1L sitz bath | Case series (low) | Dilute well; avoid open wounds |
| Probiotic yogurt | Lactobacillus, Bifidobacterium | 150ml daily oral | Meta‑analysis (moderate) | Safe for most; watch lactose |
| Chamomile tea | Bisabolol, chamazulene | Sitz bath 10min | Small trials (low‑moderate) | Possible allergen for ragweed‑sensitive |
| Sitz bath | Warm water (38-40°C) | 10min, 2-3times/day | Clinical consensus (high) | Maintain cleanliness; avoid scald |
| Psyllium husk | Soluble fiber | 1tsp in 250ml water, twice daily | RCTs (moderate) | Drink plenty of fluid; risk of blockage if dry |
| Turmeric (curcumin) | Curcumin | 500mg capsule with piperine | Meta‑analysis (moderate) | High doses may upset stomach; stop if worsening |
How to Use Natural Remedies Safely
- Start with one option. Mixing several agents can mask side‑effects and make it hard to identify the culprit if irritation occurs.
- Choose a clean, shallow basin for sitz baths; change water each session.
- For topical gels (aloe, coconut oil), apply with a sterile cotton pad after the bath, not directly onto raw ulcerated tissue.
- When ingesting supplements (probiotic yogurt, psyllium, turmeric), begin with half the suggested dose and monitor bowel habits.
- Keep a symptom diary-note pain level, frequency of bleeding, and any new reactions.
When to Seek Professional Care
Natural methods are adjuncts, not replacements for medical treatment. Call a doctor if you experience any of the following:
- Bleeding that does not stop after a few minutes.
- Fever, chills, or unexplained weight loss.
- Persistent pain lasting more than two weeks despite home care.
- Sudden worsening after starting a new remedy.
Early evaluation can uncover underlying causes such as infection, ulcerative colitis, or radiation injury that require prescription medication or procedures.
What the Research Says
Most studies on proctitis focus on pharmaceutical or surgical interventions. A handful of small trials have examined natural agents:
- A 2022 randomized trial (n=48) found that topical aloe vera reduced pain scores by 30% compared with placebo after four weeks.
- A systematic review of probiotic use in inflammatory bowel disease (including proctitis subsets) reported a modest but statistically significant reduction in disease activity indices.
- Turmeric’s curcumin exhibited anti‑inflammatory effects in animal models of colitis, but human data specific to rectal inflammation remain limited.
Overall, the evidence is promising but not definitive. The safest approach is to combine high‑quality natural options with regular medical follow‑up.
Putting It All Together: A Sample 2‑Week Plan
- Day 1-3: Begin twice‑daily sitz baths (10min) with warm water.
- Day 1-7: Add a teaspoon of psyllium husk to water, twice daily, ensuring >2L fluid intake.
- Day 4-10: After each bath, apply a thin layer of aloe vera gel.
- Day 5-14: Consume 150ml of plain probiotic yogurt each morning.
- Day 8-14: Introduce a 500mg curcumin capsule with black pepper, taken with breakfast.
- Throughout: Monitor pain, bleeding, and stool consistency; stop any remedy that causes burning.
Adjust the plan based on your comfort level and any advice from your gastroenterologist.
Frequently Asked Questions
Can I use olive oil instead of coconut oil?
Olive oil is also soothing, but coconut oil’s lauric acid has stronger antibacterial activity. If you’re allergic to coconut, extra‑virgin olive oil applied warm can be a decent alternative.
Is it safe to combine a sitz bath with apple cider vinegar?
Yes, as long as the vinegar is diluted (about 1Tbsp per litre of water). Undiluted vinegar can sting raw tissue.
How long should a sitz bath last?
Ten to fifteen minutes is sufficient. Longer soaks can dry out the skin and actually worsen irritation.
Do probiotics work for everyone with proctitis?
They help many people, especially when the gut microbiome is out of balance, but results vary. Choose a multi‑strain product with at least 10billion CFU per serving.
Should I stop my prescription meds when using natural remedies?
Never stop prescribed medication without your doctor’s approval. Natural therapies are best used as supportive measures alongside conventional treatment.
Sheila Hood
October 15, 2025 AT 21:36Alright, so you’re thinking aloe vera is a miracle cure for proctitis?
While the gel does have mild anti‑inflammatory properties, it won’t replace a prescribed steroid cream.
Start with a thin layer after a warm sitz bath and watch for any burning sensation – if it gets worse, stop immediately.
Remember, “natural” doesn’t guarantee safety; the rectal mucosa is delicate.
Use it as a supplement, not a sole treatment, and keep your doctor in the loop.
Melissa Jansson
October 16, 2025 AT 11:29Let’s dissect the pseudo‑evidence hierarchy that many of us blindly accept.
First, the term “natural” is a marketing construct engineered to exploit cognitive heuristics.
Second, the cited RCTs on aloe or coconut oil suffer from underpowered sample sizes and selection bias, rendering their p‑values practically meaningless.
Third, the mechanistic rationale-lauric acid as a bactericidal agent-fails to account for the anaerobic environment of the distal colon.
In short, the hype is disproportionate to the data, and patients deserve a more rigorous, evidence‑based protocol.
Max Rogers
October 17, 2025 AT 01:22Just a quick grammar note: when you refer to “probiotic yogurt,” treat “probiotic” as an adjective, not a noun, so it’s “probiotic yogurt,” not “probiotics yogurt.”
On the practical side, adding about 150 ml of plain, live‑culture yogurt each morning can help rebalance your gut flora without the added sugars that aggravate inflammation.
Stay consistent for at least two weeks before judging effectiveness, and keep a symptom log to track any changes.
Louie Hadley
October 17, 2025 AT 15:16I think it’s wise to keep an open mind about combining these remedies, but moderation is key.
Start with a simple sitz bath routine, then gradually introduce one supplement at a time, monitoring how your body reacts.
If you notice any increase in pain or bleeding, pull back that remedy and reassess.
This stepwise approach lets you enjoy the benefits without overwhelming the delicate rectal tissue.
Ginny Gladish
October 18, 2025 AT 05:09The data presented suffer from methodological flaws that undermine their purported efficacy.
First, sample sizes are consistently below the threshold for statistical power, inflating Type I error risk.
Second, there is a lack of blinding, introducing observer bias into subjective pain assessments.
Third, the heterogeneity of dosage forms-topical gels versus oral supplements-precludes meta‑analytic synthesis.
Consequently, any clinical recommendation based on these studies is, at best, speculative.
Faye Bormann
October 18, 2025 AT 19:02When it comes to managing proctitis, the allure of natural remedies can feel like a beacon of hope amid a sea of pharmaceuticals.
However, the romanticized view often neglects the intricate pathophysiology underlying rectal inflammation.
Aloe vera, for instance, contains aloin, which indeed possesses anti‑inflammatory properties, yet the concentration in over‑the‑counter gels varies wildly.
Coconut oil’s lauric acid exhibits antimicrobial activity, but its lipid‑rich nature can also occlude pores, potentially worsening maceration if applied excessively.
Apple cider vinegar introduces acetic acid, modestly lowering pH, yet undiluted solutions are notorious for causing burning sensations on compromised mucosa.
Probiotic yogurt offers a gentle avenue to modulate the gut microbiome, but the strains and colony‑forming units differ across brands, making standardization a challenge.
Chamomile tea, with its bisabolol content, provides soothing effects, though the evidence rests on small case series rather than robust trials.
Sitz baths remain the cornerstone because warm water improves circulation and reduces sphincter spasm, a fact supported by decades of clinical consensus.
Psyllium husk, a soluble fiber, can indeed bulk stool and reduce straining, yet inadequate fluid intake may lead to fecal impaction, counterproductive to healing.
Turmeric’s curcumin is celebrated for systemic anti‑inflammatory action, but its poor bioavailability necessitates the addition of piperine, which not everyone tolerates.
The recommended 2‑week plan wisely staggers the introduction of each agent, allowing you to isolate adverse reactions.
Nevertheless, any escalation of symptoms-especially new bleeding or fever-should prompt immediate medical evaluation.
It is also crucial to remember that "natural" does not equate to "harmless"; the rectal mucosa is particularly sensitive.
Integrating these remedies with prescribed topical steroids can be synergistic, but only under physician supervision.
Patients often overlook the importance of hygiene, which, together with a balanced diet low in irritants, forms the foundation of symptom control.
In summary, while natural options can complement conventional therapy, they are not substitutes, and their success hinges on individualized, cautious implementation.
Kathy Butterfield
October 19, 2025 AT 08:56Thanks for the concise guide! 😊
Zane Nelson
October 19, 2025 AT 22:49While the preceding analysis attempts a veneer of erudition, it ultimately skims the surface of the nuanced pharmacodynamics at play.
The reliance on buzzword-laden phrasing obscures rather than elucidates the central therapeutic mechanisms.
A more diligent exposition would reconcile the molecular pathways with clinical outcomes, rather than resorting to rhetorical flourish.
Nevertheless, the effort to interrogate the literature is commendable, albeit insufficient.
Sahithi Bhasyam
October 20, 2025 AT 12:42OMG!!! i think u r overcomplicating this!! the alove vera thing is actually simple, right?? but like, you need to be careful with dosage,, because too much can irritate,, u know?? also,, the sitz bath is like a basic thing... no need for all the fancy talk!!!
rachel mamuad
October 21, 2025 AT 02:36yeah, grammer tipz r helpful! also, the probiotic side effeects can modulate ba ctierial dysbalance, which is key in proctits. just keep an eye on daily intake and log ur symptoms for best outcomes.
Amanda Anderson
October 21, 2025 AT 16:29Honestly, reading that marathon of caution felt like a medical thriller-each sentence a plot twist where your gut could either heal or revolt!
It’s terrifying and exhilarating all at once, and now I’m both terrified and hopeful.
Carys Jones
October 22, 2025 AT 06:22It’s reprehensible that anyone would ignore the glaring methodological flaws and proclaim these “natural cures” as panaceas.
People deserve transparent, rigorously vetted treatments, not seductive pseudoscience masquerading as care.
Roxanne Porter
October 22, 2025 AT 20:16I concur with the sentiment expressed; adherence to robust clinical evidence should remain paramount.
Encouraging patients to seek validated therapies safeguards both safety and therapeutic efficacy.
Jonathan Mbulakey
October 23, 2025 AT 10:09In contemplating the balance between nature and medicine, one might reflect that healing is as much an art of patience as it is a science of intervention.
Thus, a measured approach honors both the body’s innate resilience and the clinician’s expertise.
Warren Neufeld
October 24, 2025 AT 00:02Your perspective resonates deeply; navigating chronic discomfort can feel isolating, yet embracing incremental steps often yields the most sustainable relief.
Stay compassionate with yourself as you experiment cautiously.
Deborah Escobedo
October 24, 2025 AT 13:56Great start! Remember, even small, consistent changes can add up to meaningful improvement over time.
Dipankar Kumar Mitra
October 25, 2025 AT 03:49Indeed, the cumulative effect of micro‑adjustments mirrors the butterfly effect-tiny shifts in daily habits can cascade into profound health transformations.
Don’t underestimate the power of consistency.
Tracy Daniels
October 25, 2025 AT 17:42Exactly. As you integrate these practices, keep a reflective journal to monitor progress, celebrate milestones, and adjust as needed.
Your journey can also inspire others seeking balanced, evidence‑informed pathways.