Sexual Side Effect Risk Calculator
How your medication affects sexual health
Based on clinical data from the article about sexual side effects from psychiatric medications
Your Estimated Risk
Many people start taking antidepressants or other psychiatric medications hoping to feel better-only to find their sex life has changed in ways they didn’t expect. Loss of desire, trouble getting or keeping an erection, delayed or absent orgasm, or even painful sex aren’t rare. They’re common. In fact, between 58% and 70% of people on SSRIs like sertraline or fluoxetine experience some form of sexual side effect. Yet, most never hear about this risk before they start the pill. And when they do notice something’s off, they often stay silent-out of embarrassment, shame, or the belief that nothing can be done.
Why This Isn’t Just a "Minor" Side Effect
Sexual side effects aren’t just about sex. They affect self-esteem, relationships, and whether someone sticks with their treatment. A 2003 national survey found that nearly half of men and more than 15% of women stopped taking their psychiatric meds because of sexual problems. That’s not just a personal loss-it’s a clinical failure. If someone stops their antidepressant because their libido vanished, their depression is likely to come back. And that’s worse than any side effect. The truth is, sexual dysfunction often starts before treatment. Up to half of people with untreated depression already have low desire or trouble with arousal. So when a doctor prescribes an SSRI and the patient says, "I’m not interested in sex anymore," it’s not always the medication’s fault. But it’s still the doctor’s job to sort it out.What the Medications Actually Do
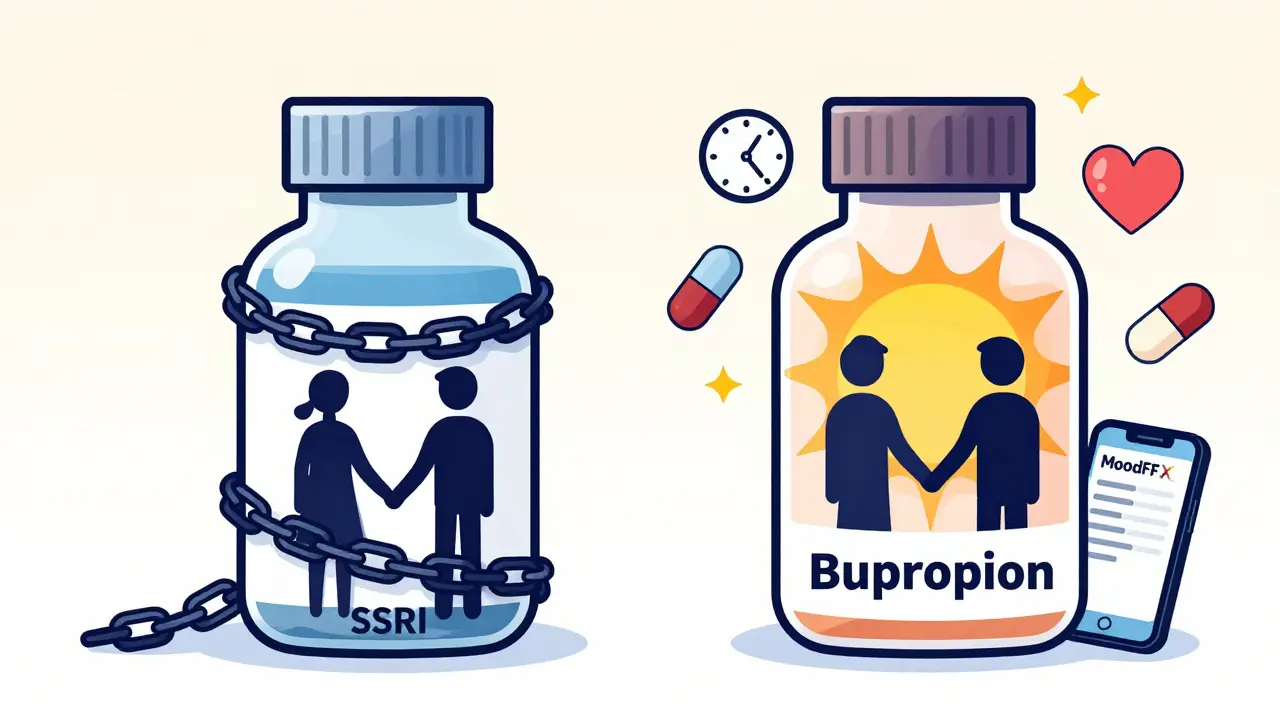
Not all drugs affect sex the same way. SSRIs-like Prozac, Zoloft, and Paxil-are the biggest offenders. They boost serotonin, which helps mood, but also shuts down sexual response pathways. About 50-70% of people on these drugs report issues. Paroxetine is the worst offender in this class. Sertraline is a bit better, but still problematic. Then there are the outliers. Bupropion (Wellbutrin) and mirtazapine (Remeron) have sexual side effect rates of just 5-10%. That’s not zero, but it’s a big difference. For people who’ve struggled with sexual side effects before, switching to one of these can be life-changing. One patient on HealthUnlocked said, "Switched to bupropion after 6 weeks. My sex life improved in two weeks. Stayed on it for 18 months." Antipsychotics like risperidone and olanzapine can raise prolactin levels, which kills libido and can cause breast milk production-even in men. Switching to aripiprazole (Abilify) fixes this in 75% of cases.What Counseling Should Look Like
Good counseling doesn’t happen after the problem shows up. It starts before the first pill is taken. The best approach has four parts:- Baseline check: Ask about sexual function before starting medication. Tools like the Arizona Sexual Experience Scale (ASEX) take less than 7 minutes. It’s not about being invasive-it’s about knowing what’s normal for you.
- Clear warning: "This medication can affect your sex life. It happens to 6 out of 10 people. It doesn’t mean something’s wrong with you. And there are ways to fix it." Normalizing the issue reduces shame and increases reporting.
- Follow-up schedule: Don’t wait for the patient to bring it up. Check in at 2, 4, and 6 weeks. A 2022 study showed that structured follow-up reduces self-discontinuation by 32%.
- Contingency plan: "If this happens, here’s what we can do: adjust the dose, switch meds, add sildenafil, or try timing sex around your dose. We’ve got options."
What Actually Works to Fix It
There’s no one-size-fits-all fix. But here’s what the data says works:- Dose reduction: Works for 25-30% of people. Sometimes taking half the dose still controls depression but spares your sex life.
- Drug holidays: Skipping your pill for 2-3 days before planned sex helps 40% of people. But it’s risky with short-acting drugs like paroxetine-relapse rates hit 15%.
- Switching meds: Going from an SSRI to bupropion or mirtazapine works in 65-70% of cases. This is often the best long-term solution.
- Phosphodiesterase-5 inhibitors: Viagra, Cialis, and similar drugs help with erections in 55-60% of men. But they do almost nothing for delayed orgasm or low desire. And if you don’t know how to use them properly, they won’t work. One doctor says most treatment failures come from patients taking them wrong.
- Couples therapy: If the side effect has caused tension in your relationship, therapy helps 50% of couples. Sex isn’t just physical-it’s emotional. When one partner feels broken or guilty, it changes how both of them connect.
- Sexual scheduling: Timing sex for when the drug’s effects are lowest (like right after waking up, before the daily dose) helps 35% of people.
Why So Many People Stay Silent
On Reddit’s r/mentalhealth, 68% of 1,247 respondents said their doctor never mentioned sexual side effects before prescribing. That’s not negligence-it’s silence. And silence kills adherence. People don’t report these issues because:- They think it’s normal or "just part of getting better."
- They’re embarrassed to talk about it.
- They assume their doctor won’t care or won’t have a solution.
- They’ve been dismissed before.
Who’s Missing From the Conversation
Most research on sexual side effects focuses on cisgender men. But women experience these problems too-often differently. About 57% report low desire. 38% have pain during sex. 30% can’t orgasm. Yet only 12% of clinical trials on sexual dysfunction include enough female participants to draw solid conclusions. LGBTQ+ patients face even bigger gaps. A 2022 study found they’re 28% less likely to have sexual side effects discussed with them. Doctors assume their sexual needs are different-or don’t exist. That’s not just inaccurate. It’s harmful.
What’s Changing
The tide is turning. The American Psychiatric Association’s 2023 guidelines now include a dedicated section on sexual side effect management. Major health systems are rolling out screening protocols. Telehealth services like Ro and Hims are seeing 45% of their consultations relate to medication-induced sexual dysfunction. New tools are emerging too. The MoodFX app lets patients track mood and sexual function together. Over 127,000 people are using it. And a new drug, a 5-HT2C receptor antagonist, is in phase 3 trials-designed to reverse SSRI-induced sexual dysfunction without hurting the antidepressant effect. Results are expected in mid-2024.What You Can Do
If you’re on medication and something’s off:- Don’t wait. Don’t assume it’ll go away.
- Write down what’s changed: desire? arousal? orgasm? pain?
- Bring it up at your next appointment. Say: "I’ve noticed changes in my sex life since starting this med. What can we do?"
- Ask: "Is there another medication with fewer sexual side effects?"
- Ask: "Can we try a lower dose?"
- Ask: "Can you refer me to someone who helps with sexual health and meds?"
- Start the conversation before prescribing.
- Use a simple tool like ASEX.
- Don’t say, "It’s just part of treatment." Say, "This happens often, and we can fix it."
- Have a plan ready: dose tweak, switch, add-on, or referral.
- Train your team. Pharmacists can help too.
It’s Not Just About Sex
Sexual side effects are a symptom of a bigger problem: we treat mental health like it’s only about mood. But recovery isn’t just about feeling less sad. It’s about feeling whole again-connected, desired, alive. If your treatment takes away your ability to be intimate, you haven’t healed. You’ve just traded one pain for another. The good news? We know how to fix this. We’ve had the tools for years. What’s missing is the courage to talk about it-and the system to make it routine.Do all antidepressants cause sexual side effects?
No. SSRIs like fluoxetine and sertraline cause sexual side effects in 50-70% of users. But bupropion (Wellbutrin) and mirtazapine (Remeron) have rates as low as 5-10%. Not all antidepressants are the same-some are much gentler on sexual function.
Can I just stop taking my medication if sex life is affected?
Stopping suddenly can cause withdrawal symptoms or make depression worse. Instead, talk to your provider. There are safer options: lowering the dose, switching medications, or adding a short-term fix like sildenafil. Never stop without medical guidance.
How long do sexual side effects last after stopping the medication?
For most people, sexual function returns within a few weeks after stopping the drug. But in rare cases, especially with long-term SSRI use, symptoms can persist for months or longer-a condition called Post-SSRI Sexual Dysfunction (PSSD). It’s uncommon, but real. If symptoms don’t improve after 2-3 months off the drug, see a specialist.
Can counseling or therapy help with sexual side effects?
Yes. Couples therapy helps 50% of people whose relationships have been strained by sexual side effects. Individual sex therapy can also help rebuild confidence and explore new ways to connect. Therapy doesn’t replace medical solutions, but it supports emotional recovery.
Is it normal to feel embarrassed talking about this with my doctor?
Yes, it’s very common. But it’s also unnecessary. Doctors see this every day. The more people speak up, the more normal it becomes. Your provider can’t help if they don’t know. Saying, "I’ve noticed changes in my sex life," opens the door to real solutions.
Are there any new treatments coming for medication-induced sexual dysfunction?
Yes. A new drug targeting the 5-HT2C receptor is in phase 3 trials and could reverse sexual side effects without reducing antidepressant effectiveness. Results are expected in mid-2024. Also, digital tools like the MoodFX app now let patients track sexual function alongside mood, helping both patient and provider make better decisions.

Ashley Karanja
January 26, 2026 AT 05:12Let’s be real-this isn’t just about libido or erectile function. It’s about the erosion of intimacy, the quiet loneliness that creeps in when your body no longer feels like yours. SSRIs don’t just dampen desire-they dampen the *story* you tell yourself about being desirable, about being whole. And when doctors treat this like a footnote, they’re not just neglecting physiology-they’re neglecting identity. We need to stop pathologizing the side effect and start normalizing the conversation. This isn’t weakness. It’s biology meeting bureaucracy.
And for the love of all that’s neurochemical, let’s stop pretending bupropion is a magic bullet. It helps some, sure, but it’s not a cure-all. We need a spectrum of solutions, not a single alternative.
Also, PSSD isn’t rare. It’s underreported. Because people think they’re crazy when they still can’t come six months after quitting. They’re not. The science is just catching up.
Emotional intimacy isn’t restored by a pill. It’s restored by someone saying, ‘I see you, and I’m not leaving.’
George Rahn
January 26, 2026 AT 12:31One must ask: is the modern psychiatric paradigm not fundamentally flawed if it routinely sacrifices the erotic self on the altar of mood stabilization? We medicate the mind into a numb cathedral and wonder why the soul refuses to sing. The pharmaceutical industry has commodified serotonin, yet refuses to acknowledge that human sexuality is not a malfunction to be corrected, but a sacred rhythm to be honored.
And yet-here we are, prescribing antidepressants like they’re multivitamins, while the patient’s capacity for pleasure becomes collateral damage. This is not medicine. It is moral negligence dressed in white coats.
Let us not confuse symptom suppression with healing. A man who cannot feel desire is not cured-he is hollowed.
And to those who say, ‘Just switch meds’-have you ever tried explaining to your partner that your love is now pharmacologically mediated? That your arousal is scheduled like a dentist appointment? That’s not treatment. That’s existential exile.
Karen Droege
January 27, 2026 AT 00:25Okay, but can we talk about how women are just… ignored in this whole conversation? Like, yes, men get the Viagra talk, but women? We get ‘it’s probably depression’ or ‘try more foreplay.’
I was on sertraline for 18 months. Zero libido. Zero arousal. Zero orgasm. And my psychiatrist said, ‘Maybe you’re just not attracted to your husband anymore.’
Welp. I divorced him. And then I found a therapist who actually knew what ASEX was. And switched to mirtazapine. And now? I can feel my body again. Not because I ‘fixed’ myself-but because someone finally *listened*.
Also-couples therapy isn’t a luxury. It’s a necessity. When your partner thinks your lack of desire means you don’t love them? That’s trauma. Not biology.
And yes, PSSD is real. I know women who still can’t orgasm 3 years later. No one talks about it. That’s the real scandal.