Medication-Citrus Interaction Checker
Check Your Medication Safety
Enter your medication and citrus fruit to see if it's safe to consume together. Includes pomelo and Seville orange risks not covered by standard warnings.
Select medication and citrus fruit to see results
Most people know grapefruit can mess with their meds. But what about the big, pinkish fruit at the Asian grocery that looks like a grapefruit but is way bigger? Or the bitter orange marmalade your grandma swears by? These aren’t just exotic snacks-they’re hidden risks if you’re on certain prescriptions.
What Makes Pomelo and Seville Orange Different?
Pomelo (Citrus maxima) is the giant of the citrus family. It can weigh up to 2 pounds, has thick rind, and flesh that ranges from pale yellow to deep pink. It’s sweet but slightly tart, popular in Southeast Asia and increasingly found in U.S. supermarkets. Seville orange (Citrus aurantium), on the other hand, is too bitter to eat raw. You’ll find it in Spanish marmalades, some cocktails, and traditional remedies. Both are not just cousins to grapefruit-they’re more potent.Here’s the catch: they contain the same chemicals that make grapefruit dangerous with meds-furanocoumarins like bergamottin and 6’,7’-dihydroxybergamottin. These compounds shut down enzymes in your gut that normally break down drugs before they enter your bloodstream. When those enzymes are blocked, your body absorbs way more of the drug than intended. For some medications, that’s the difference between healing and hospitalization.
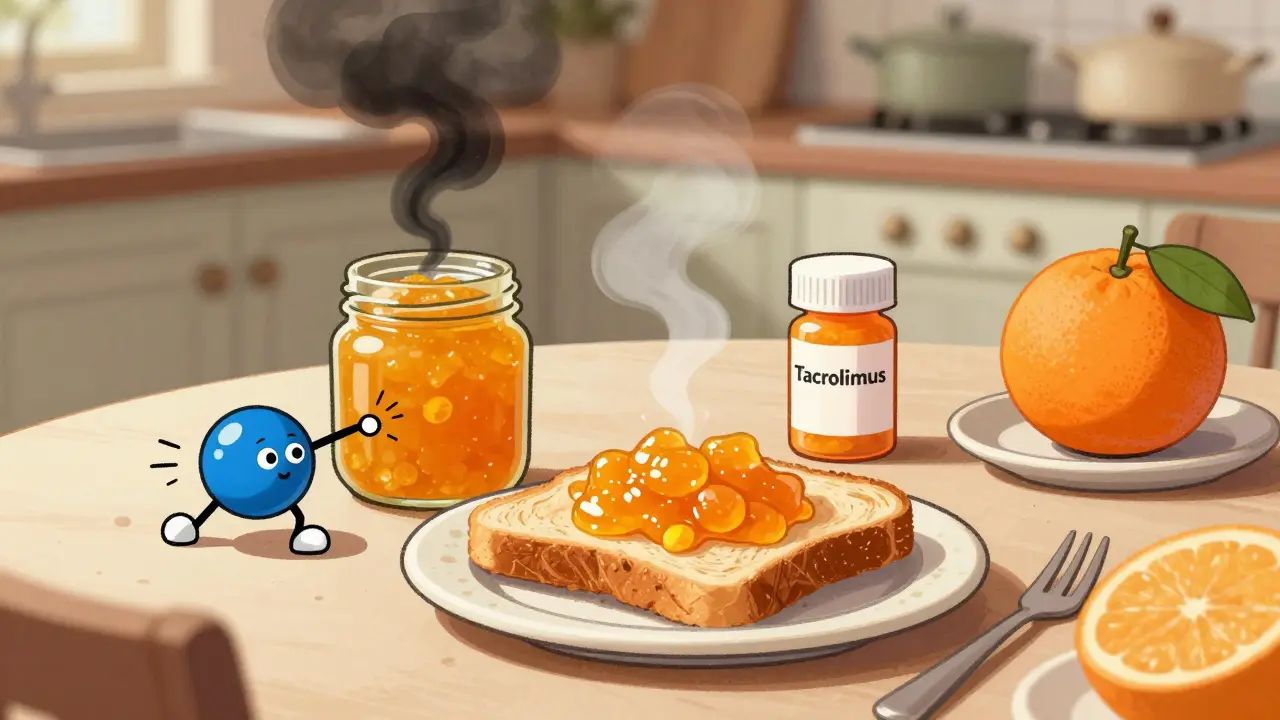
Studies show pomelo has 20-30% more of these inhibitors than grapefruit. Seville orange peel-used in marmalade-can contain up to 4.0 μM of bergamottin, compared to grapefruit’s 2.0 μM. That’s not a small difference. It means even a spoonful of Seville orange marmalade on toast could be enough to spike your drug levels.
Which Medications Are at Risk?
Not all drugs are affected. The danger is focused on ones that rely on the CYP3A4 enzyme and OATP transporters to be processed. If your med falls into one of these categories, pomelo and Seville orange are off-limits:- Statins (like simvastatin, atorvastatin): These lower cholesterol. Too much in your system can cause rhabdomyolysis-a condition where muscle breaks down, damaging kidneys. A 2018 study found pomelo increased simvastatin levels by 350%, worse than grapefruit’s 300%.
- Calcium channel blockers (like amlodipine, felodipine): Used for high blood pressure. Extra drug can drop your blood pressure dangerously low, causing dizziness, fainting, or even heart issues.
- Immunosuppressants (like tacrolimus, cyclosporine): Critical for transplant patients. Too much can poison your kidneys or liver. One case report showed tacrolimus levels jumped 400% after Seville orange marmalade.
- Benzodiazepines (like midazolam, triazolam): Used for anxiety or sleep. Higher levels mean extreme drowsiness, slowed breathing, or coma.
- Some anti-arrhythmics (like amiodarone): Can trigger dangerous heart rhythms.
Drugs like metformin, ibuprofen, or most antibiotics? No problem. The risk is narrow but deadly. If you’re on any of these, don’t assume grapefruit is the only culprit.
How Long Does the Effect Last?
This is where most people get it wrong. You don’t just need to avoid these fruits the day you take your pill. The enzyme inhibition is irreversible. Once CYP3A4 is blocked, your body has to make new enzymes to replace them. That takes about 72 hours.So if you eat a slice of pomelo on Monday, your system is still vulnerable on Thursday. Even if you take your medication on Friday, the risk remains. That’s why the FDA recommends avoiding these fruits for at least three days before and during treatment with sensitive drugs.
And it’s not just juice. Eating the fruit, drinking tea made from the peel, or even using citrus-flavored supplements can trigger the same reaction. One patient in a 2022 Reddit thread described rhabdomyolysis after eating pomelo daily for two weeks-no juice, just the flesh. No one warned him.
Why Is This So Overlooked?
Grapefruit gets all the attention. But here’s the truth: only 37% of pomelo and Seville orange products carry any warning label. Compare that to 78% for grapefruit. Most people don’t know Seville orange is different from sweet orange. They see “orange marmalade” and assume it’s safe.Pharmacists are better off than most, but still lag. A 2023 survey found only 42% of community pharmacists routinely ask patients about pomelo or Seville orange use. Most still just ask, “Do you eat grapefruit?”
And it’s not just patients. Doctors often don’t know either. A 2021 JAMA Internal Medicine editorial pointed out that many clinicians think these interactions are rare or overblown. But data from the FDA’s Adverse Event Reporting System shows pomelo and Seville orange account for 15% of all citrus-drug interaction cases between 2015 and 2022. That’s not rare. That’s significant.
Real Stories, Real Consequences
A transplant patient in North Carolina ended up in the ER after eating Seville orange marmalade every morning for a month. His tacrolimus levels were off the charts. He nearly lost his new kidney. Another man in Florida, on simvastatin, started eating pomelo because he thought it was “healthier than grapefruit.” Two weeks later, he couldn’t walk. His muscles were breaking down. His creatine kinase levels were 20 times higher than normal. These aren’t outliers. They’re predictable. And they’re preventable.On the flip side, patients who switch to sweet oranges (like navel or Valencia) report zero issues. A 2022 Mayo Clinic survey found 82% of people who made the switch felt confident and safe. Sweet oranges don’t contain furanocoumarins. They’re the safe alternative.
What Should You Do?
If you’re on medication:- Check your prescription label. If it says “avoid grapefruit,” assume pomelo and Seville orange are also off-limits.
- Ask your pharmacist or doctor. Don’t assume they know. Say: “I’ve heard pomelo and Seville orange can interact with meds too. Should I avoid those?”
- Read labels on marmalades and juices. If it says “Seville orange” or “bitter orange,” put it back. Even “natural flavoring” from these fruits can be risky.
- When in doubt, choose sweet oranges. Navel, Valencia, blood orange-these are safe. They don’t block the enzymes.
- Wait 72 hours. If you accidentally eat one of these fruits, don’t take your medication until three days have passed.
And if you’re a caregiver or family member: watch what’s on the table. A jar of marmalade or a bowl of pomelo might seem harmless. But if someone’s on a statin or transplant drug, it’s a silent threat.
What’s Changing?
The FDA is finally catching up. In 2023, they proposed expanding warning labels to include all furanocoumarin-containing citrus fruits-not just grapefruit. The rule is expected to go into effect by mid-2025. Until then, the burden is on you.Research is also accelerating. The University of Washington just got $2.1 million from the NIH to study pomelo interactions in detail. And electronic health records are slowly starting to flag these risks. But right now, you’re your own best defense.
Bottom Line
Pomelo and Seville orange aren’t just fancy fruits. They’re drug interaction powerhouses-sometimes stronger than grapefruit. If you’re on statins, blood pressure meds, or immunosuppressants, treat them like the hazard they are. Don’t wait for a warning label. Don’t assume “it’s just an orange.” Your life might depend on knowing the difference.Can I eat sweet oranges if I’m on medication?
Yes. Sweet oranges like navel, Valencia, or blood oranges do not contain furanocoumarins and are safe to eat with most medications. They’re the best citrus alternative if you’re avoiding grapefruit, pomelo, or Seville orange.
Is pomelo juice worse than grapefruit juice?
In many cases, yes. Studies show pomelo juice contains higher levels of furanocoumarins-up to 30% more than grapefruit juice. One study found it increased simvastatin levels by 350%, compared to 300% for grapefruit. The risk is similar, but often greater.
Does cooking or baking with Seville orange destroy the interaction risk?
No. Furanocoumarins are heat-stable. Making marmalade, jam, or baking with Seville orange doesn’t break them down. The risk remains even in cooked products. If the fruit is in the recipe, the interaction risk is still there.
I ate pomelo and took my pill the next day. Should I be worried?
Yes. The enzyme inhibition lasts up to 72 hours. Even if you ate pomelo 24 hours before your dose, your body may still be unable to metabolize the drug properly. Wait three full days before taking medications known to interact with citrus fruits.
Are there any citrus fruits that are completely safe?
Sweet oranges (navel, Valencia), tangerines, clementines, and mandarins are safe. Lemons and limes have very low levels of furanocoumarins and are generally considered low risk, but it’s still best to avoid large amounts if you’re on a sensitive medication. Stick to sweet oranges for the safest option.
