Standing up from a chair and feeling dizzy? For many older adults on blood pressure medication, this isn’t just a minor inconvenience-it’s a real danger. Orthostatic hypotension, a sudden drop in blood pressure when standing, is one of the most common and underrecognized side effects of hypertension treatment in seniors. It doesn’t just cause lightheadedness. It leads to falls, fractures, hospitalizations, and even death. The scary part? Many doctors and patients still believe that lowering blood pressure too much causes this problem. The truth is more complex-and more hopeful.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension happens when your systolic blood pressure drops by 20 mm Hg or more, or your diastolic pressure drops by 10 mm Hg or more, within three minutes of standing up. It’s not just a quick dizzy spell. It’s a measurable, dangerous physiological event. In older adults with high blood pressure, it affects between 3% and 26% of people, depending on age, medications, and other health conditions. The risk climbs sharply after age 70. Why? Because aging weakens the body’s natural ability to adjust blood pressure quickly. Baroreceptors-your body’s pressure sensors-don’t respond as fast. Blood vessels don’t constrict as well. The heart doesn’t pump as efficiently. And the kidneys produce less of the hormones that help regulate pressure.Which Blood Pressure Medications Carry the Highest Risk?
Not all antihypertensive drugs are created equal when it comes to orthostatic risk. Some are far more likely to trigger drops in blood pressure upon standing.- Alpha blockers (like doxazosin, terazosin): These have the highest risk. Up to 28% of older adults taking them experience orthostatic hypotension. They relax blood vessels too aggressively, especially when standing.
- Beta-blockers (like metoprolol, atenolol): These slow the heart rate and reduce cardiac output. Studies show they nearly triple the risk of sustained low blood pressure when standing. Odds ratio: 3.36.
- Diuretics (like hydrochlorothiazide, furosemide): By reducing fluid volume, they can make blood pressure too low when upright. Risk increases with dehydration or excessive dosing.
- Central sympatholytics (like clonidine): These suppress the nervous system’s ability to raise blood pressure. Often prescribed for sleep or anxiety, they’re dangerous in seniors with hypertension.
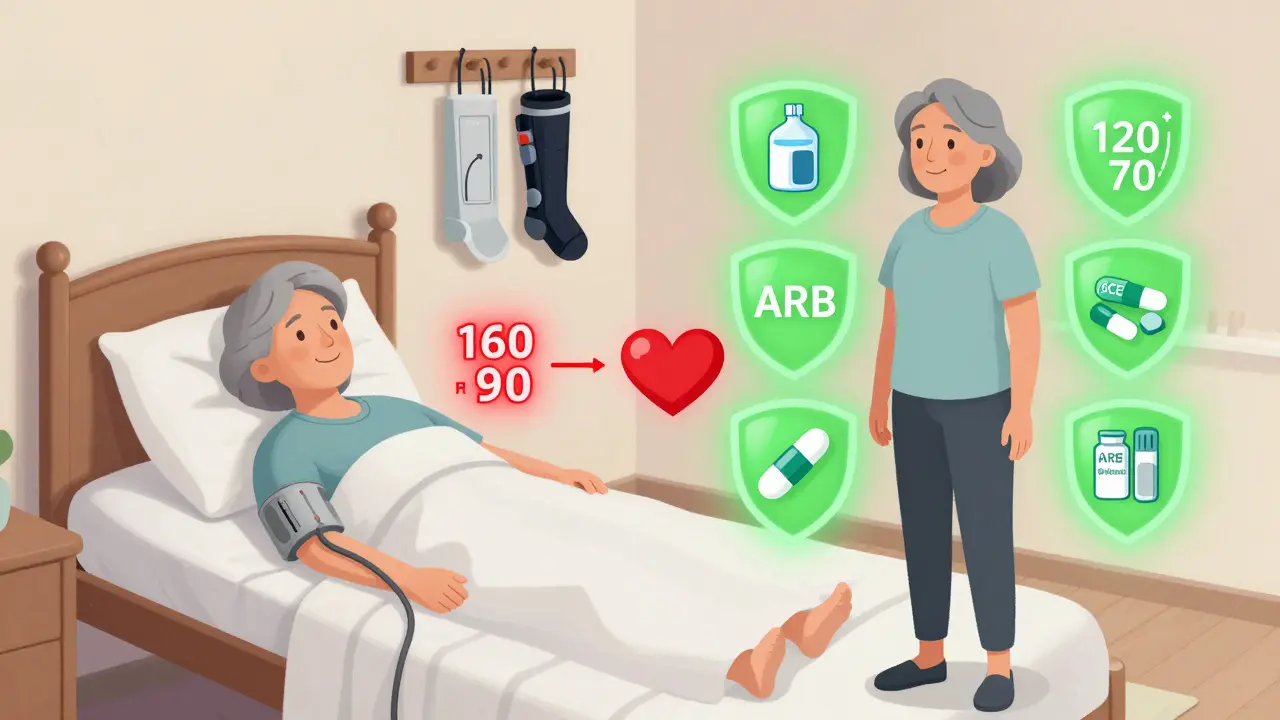
On the flip side, two classes of drugs stand out for their safety:
- ACE inhibitors (like lisinopril) and ARBs (like losartan): These show the lowest risk. Multiple studies report a 14-15% reduction in orthostatic hypotension compared to other classes. Some even suggest they help protect against it.
- Calcium channel blockers: Not all are the same. Amlodipine and isradipine have very low risk due to their slow, gentle action on blood vessels. Diltiazem and verapamil, however, carry higher risk because of how they’re metabolized in older livers.
Here’s the key takeaway: It’s not the goal of lowering blood pressure that causes orthostatic hypotension-it’s the wrong drugs doing it too fast.
The Myth of "Too Much Blood Pressure Lowering"
For years, doctors were told: "Don’t treat older adults too aggressively. They’ll get dizzy and fall." But the SPRINT trial changed everything. This massive study followed nearly 10,000 adults over 50 with high blood pressure. One group aimed for a systolic pressure below 120 mm Hg. The other aimed for below 140 mm Hg. The intensive group had no higher rate of orthostatic hypotension. In fact, they had slightly lower rates (14.5% vs. 14.7%). And they had 25% fewer heart attacks, strokes, and heart failure events.A follow-up analysis of nine other trials involving over 18,000 people confirmed it: more aggressive blood pressure control actually reduced orthostatic hypotension risk by 17%. Why? Because better overall vascular health improves the body’s ability to adapt. The problem isn’t the target-it’s the medication choice and timing.
When to Consider Stopping or Switching Medications
If an older adult is dizzy when standing, the instinct is often to cut back on meds. But that’s often the wrong move. As Dr. Harry Goldblatt from Case Western Reserve University explains, "The danger isn’t the standing blood pressure-it’s the supine (lying down) pressure." If you lower meds to fix dizziness, you might leave the patient with dangerously high pressure while lying down, increasing stroke risk.Instead, follow this practical approach:
- Identify high-risk drugs. Look for alpha blockers, beta-blockers, diuretics, or central sympatholytics. These are the usual suspects.
- Test before and after. Measure blood pressure lying down and standing. If the drop is over 20/10 mm Hg and the person has symptoms, it’s likely medication-related.
- Switch, don’t just stop. Replace a high-risk drug with a safer alternative. For example, swap doxazosin for losartan. Or switch metoprolol to amlodipine.
- Go slow. Change one medication at a time. Wait 2-4 weeks between changes. Monitor both lying and standing pressures weekly.
Studies show that when patients switch from high-risk to low-risk medications, about 65% report fewer dizziness episodes and fewer falls within a month.
Non-Medication Strategies That Work
Medication changes are important-but they’re not the whole story. Simple, daily habits can make a huge difference.- Stand up slowly. Don’t jump out of bed. Sit on the edge for 30 seconds. Then stand for another 30 seconds before walking.
- Hydrate well. Drink 16-20 ounces of water before getting up in the morning. Water boosts blood volume and helps maintain pressure.
- Avoid large meals. Blood pools in the gut after eating, lowering pressure. Eat smaller meals more often.
- Wear compression stockings. These help push blood back up from the legs. They’re especially helpful after sitting for long periods.
- Don’t stand still. If you’re standing in line, shift your weight or march in place. Movement keeps blood flowing.
- Raise the head of the bed. Elevating the head 6-10 inches at night reduces nighttime drops in pressure and helps reset the system.
These aren’t "nice-to-haves." They’re essential. Patients who practice these habits daily see measurable improvement in 2-4 weeks.

What About Medications to Treat Orthostatic Hypotension?
Sometimes, even after switching antihypertensives, symptoms persist. In those cases, doctors may consider adding medications specifically designed to raise standing blood pressure:- Midodrine (Orvaten): A vasoconstrictor that tightens blood vessels. Works quickly but can cause high lying-down pressure. Use with caution.
- Droxidopa (Northera): Converts to norepinephrine, boosting pressure. Requires careful monitoring.
- Fludrocortisone: A steroid that helps retain salt and water. Can cause swelling or heart strain.
- Pyridostigmine (Mestinon): Improves nerve signaling to blood vessels. Less commonly used but helpful in some cases.
These aren’t first-line. They’re for when lifestyle and medication changes aren’t enough. And they come with their own risks. Always start low and go slow.
The Bigger Picture: Why This Matters Now
About 74.5 million Americans over 65 have high blood pressure. Based on current data, 2.2 to 19.4 million of them likely have orthostatic hypotension. That’s up to one in four seniors on blood pressure meds. And it’s not just about falls. It’s about independence. It’s about avoiding nursing homes. It’s about living without fear.Prescribing trends are shifting. In 2023, 38% of new hypertension prescriptions for seniors were ACE inhibitors or ARBs-up from 32% in 2020. Why? Because doctors are learning that safety isn’t about lowering pressure less-it’s about lowering it smarter.
The American Geriatrics Society’s 2023 Beers Criteria now lists alpha blockers and certain beta-blockers as "potentially inappropriate" for older adults with orthostatic risk. That’s a big deal. It’s changing how thousands of prescriptions are written every week.
And the future? Researchers are testing "smart" blood pressure pills that only activate when you stand up. Two are already in Phase II trials. That’s not science fiction-it’s the next step.
What Should Seniors and Families Do?
If you or a loved one is on blood pressure medication and has felt dizzy when standing:- Don’t ignore it. Dizziness isn’t "just part of aging." It’s a warning sign.
- Track symptoms. Note when it happens: after standing? After meals? After taking medication?
- Ask for a standing BP check. Request that your doctor measure blood pressure lying down and standing at your next visit.
- Ask about medication alternatives. "Is there a safer option than what I’m on?" is a powerful question.
- Start the habits. Drink water first thing in the morning. Stand up slowly. Wear compression socks if recommended.
You don’t need to stop your medication. You don’t need to live in fear. You just need to know what’s happening-and what to ask for.
Can blood pressure medication cause dizziness when standing?
Yes, certain blood pressure medications can cause dizziness when standing due to orthostatic hypotension. This is a drop in blood pressure that happens when moving from lying or sitting to standing. Medications like alpha blockers, beta-blockers, diuretics, and central sympatholytics are most likely to cause this. ACE inhibitors and ARBs carry much lower risk and may even help prevent it.
Should I stop my blood pressure medicine if I get dizzy?
No, don’t stop your medication on your own. Stopping abruptly can cause your blood pressure to spike while lying down, which increases stroke risk. Instead, talk to your doctor. They can check your blood pressure in different positions and switch you to a safer medication if needed. The goal is to control high blood pressure without causing low pressure when standing.
What’s the safest blood pressure medicine for older adults?
ACE inhibitors (like lisinopril) and ARBs (like losartan) are generally the safest for older adults at risk of orthostatic hypotension. They have the lowest association with dizziness and falls. Among calcium channel blockers, amlodipine and isradipine are preferred over diltiazem or verapamil. Avoid alpha blockers like doxazosin and certain beta-blockers like metoprolol if dizziness is an issue.
Can lifestyle changes help with dizziness from blood pressure meds?
Yes, lifestyle changes can significantly reduce dizziness. Drink a glass of water before getting up. Stand up slowly-sit on the edge of the bed for 30 seconds first. Wear compression stockings. Avoid large meals. Raise the head of your bed slightly. These habits help your body adjust to standing and can reduce symptoms within weeks.
Is it dangerous to have low blood pressure when standing?
Yes, it can be. A sudden drop in blood pressure upon standing can cause fainting, falls, fractures, and head injuries. In older adults, falls are a leading cause of hospitalization and death. Even if you don’t faint, repeated episodes of dizziness can lead to fear of movement, reduced activity, muscle loss, and increased risk of disability. It’s not just about the moment-it’s about long-term safety.
How often should older adults have their blood pressure checked in different positions?
Anyone over 65 on blood pressure medication should have their blood pressure checked both lying down and standing at least once a year. If they’ve had dizziness, falls, or a recent medication change, it should be checked every 2-4 weeks for the first few months. Doctors should make this a routine part of care-it’s not optional.

Iona Jane
January 16, 2026 AT 02:58Jaspreet Kaur Chana
January 17, 2026 AT 06:15Nishant Garg
January 18, 2026 AT 00:41Sarah Mailloux
January 18, 2026 AT 15:53Amy Ehinger
January 19, 2026 AT 17:53Tom Doan
January 20, 2026 AT 06:16Sohan Jindal
January 22, 2026 AT 04:06Arjun Seth
January 22, 2026 AT 07:59Mike Berrange
January 24, 2026 AT 01:16Dan Mack
January 24, 2026 AT 02:53Amy Vickberg
January 25, 2026 AT 12:56