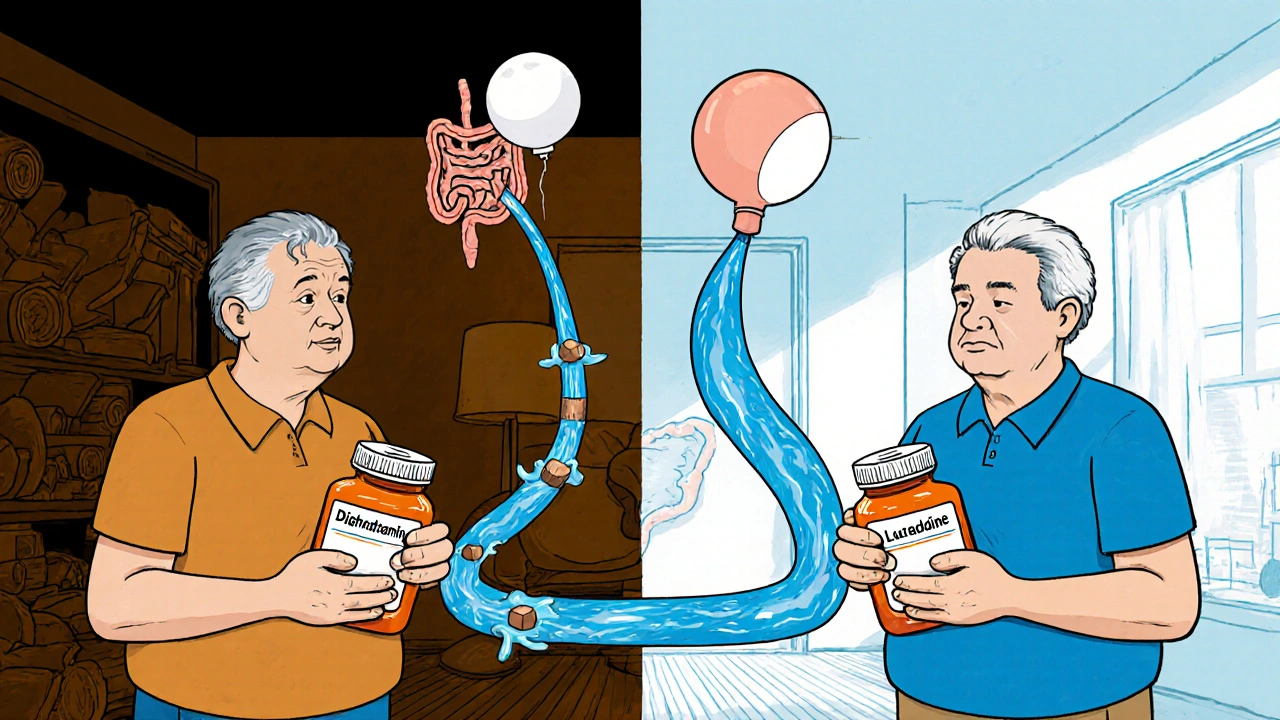
Most people reach for antihistamines when their allergies flare up - sneezing, itchy eyes, runny nose. But few realize that the pill they swallow might be silently disrupting their bladder, gut, and saliva production. First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and promethazine don’t just block histamine. They also shut down acetylcholine, a key messenger in your nervous system. This unintended effect - called anticholinergic activity - is why so many users report dry mouth, constipation, and trouble peeing. And it’s not just uncomfortable. For older adults, these side effects can be dangerous.
How Antihistamines Cause Dry Mouth
Your saliva doesn’t just help you chew and swallow. It protects your teeth, prevents infections, and keeps your mouth from feeling like sandpaper. When you take a first-generation antihistamine, it blocks M3 receptors in your salivary glands. These receptors normally tell your body to make saliva. When they’re turned off, saliva production drops by 60-70%. That’s not just a nuisance - it’s a health risk.People who use diphenhydramine regularly often describe it as a constant need to sip water, even at night. One 72-year-old woman from Bristol told her pharmacist she’d started sleeping with a glass of water by her bed after years of waking up with a throat so dry she couldn’t swallow. That’s not dehydration. That’s pharmacology.
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) barely touch these receptors. Clinical trials show dry mouth affects only 2-4% of users with these drugs, compared to nearly 30% with diphenhydramine. If you’re constantly reaching for gum or mouth spray after taking an allergy pill, you’re probably on the wrong one.
Why Constipation Comes With Your Allergy Pill
Your gut moves because acetylcholine tells the muscles to contract. Antihistamines like diphenhydramine interfere with that signal, slowing down digestion. Studies show this reduces gut motility by 30-40% and doubles the time food takes to pass through. The result? Constipation that lasts days.It’s not just about being “regular.” In older adults, especially those with existing bowel issues, this can lead to fecal impaction - a serious condition requiring medical intervention. A 2020 study in the Journal of the American Geriatrics Society found that 15-20% of elderly patients on first-generation antihistamines developed constipation severe enough to require laxatives. Only 3-5% of those on second-generation options did.
One man in his late 60s in Bristol switched from Benadryl to loratadine after spending three days in the ER with a bowel obstruction. He’d been taking diphenhydramine every night for years, thinking it helped him sleep. He didn’t realize his constipation was drug-induced. After switching, his bowel movements returned to normal within a week.
Urinary Retention: A Silent Risk for Men and Older Adults
If you’re male and over 50, or if you’ve ever had trouble starting your stream or feeling like you didn’t fully empty your bladder, first-generation antihistamines can make it worse - sometimes dangerously so. These drugs block M2 and M3 receptors in the bladder wall and urethral sphincter. That weakens bladder contractions and tightens the sphincter, making it hard to pee.Research from the Journal of Urology shows that first-generation antihistamines reduce bladder contraction force by 25-35%. In men with enlarged prostates, this can trigger acute urinary retention - a medical emergency requiring catheterization. A 2022 study found that 31% of men with moderate to severe prostate symptoms developed full urinary retention within 48 hours of taking diphenhydramine.
Even women aren’t immune. Older women with weak bladder muscles or pelvic floor issues can experience similar problems. The American Urological Association recommends avoiding first-generation antihistamines entirely in anyone with an International Prostate Symptom Score above 8. That’s not a suggestion. It’s a warning.
Why Second-Generation Antihistamines Are Safer
The newer antihistamines - cetirizine, loratadine, fexofenadine, and levocetirizine - were designed to stay out of the brain and away from acetylcholine receptors. They bind to histamine receptors with high precision but barely interact with muscarinic ones. Their Ki values (a measure of binding strength) for M1 receptors are over 1,000 nM, compared to just 87 nM for diphenhydramine. That’s more than 10 times less likely to cause anticholinergic effects.Real-world data backs this up. A 2021 study in Annals of Allergy, Asthma & Immunology showed:
- Dry mouth: 28% with diphenhydramine vs. 4% with cetirizine
- Constipation: 18% vs. 4%
- Urinary retention: 7% vs. 0.8%
And it’s not just about side effects. Second-generation antihistamines last 24 hours. You take one pill a day. First-generation ones wear off in 4-6 hours, meaning you’re tempted to take more - which only makes the anticholinergic burden worse.
The Hidden Risk: Cognitive Decline and Dementia
Dry mouth and constipation are annoying. But what happens when your brain starts to feel foggy? That’s not just aging. It’s the anticholinergic effect.Dr. Shelley Gray’s landmark 2015 study in JAMA Internal Medicine followed 3,434 older adults for seven years. Those who took first-generation antihistamines daily had a 54% higher risk of developing dementia. For every extra year they used more than 90 doses, their risk went up another 20%. Diphenhydramine has the highest possible anticholinergic cognitive burden score - 3.0 - meaning it’s among the most damaging drugs for memory.
The American Geriatrics Society’s Beers Criteria lists first-generation antihistamines as “potentially inappropriate” for people over 65. The European Academy of Allergy and Clinical Immunology says to avoid them entirely in this group. Mayo Clinic stopped using diphenhydramine in hospitals in 2022 because it was causing delirium in older patients.
It’s not just about memory. Falls risk increases by 34% with even short-term use. Sedation plus poor bladder control plus dizziness equals a higher chance of breaking a hip. And once that happens, recovery is rarely complete.
What to Do Instead
If you’re currently using diphenhydramine, chlorpheniramine, or promethazine for allergies or sleep, here’s what to do:- Switch to a second-generation antihistamine: cetirizine, loratadine, or fexofenadine. They work just as well for allergies - without the dry mouth, constipation, or urinary issues.
- Check your medicine cabinet. Many sleep aids, cold meds, and motion sickness pills still contain diphenhydramine. Read the labels. “Nighttime” doesn’t mean “safe.”
- If you have an enlarged prostate, bladder issues, or constipation, avoid first-generation antihistamines entirely. Talk to your doctor about alternatives.
- For dry mouth: chew sugar-free gum with xylitol. It boosts saliva by 40-60% within minutes.
- For constipation: try 17g of polyethylene glycol daily if you must use a first-generation drug. It cuts constipation risk from 18% to 5%.
Don’t assume your doctor knows you’re taking these. Many people don’t think of over-the-counter pills as “medications.” But they’re drugs - with real side effects.
Market Shifts and Regulatory Warnings
The tide is turning. The FDA added a dementia risk warning to diphenhydramine labels in 2021. The European Medicines Agency banned first-generation antihistamines for children under 2 in 2020. In the U.S., Medicare now requires special justification to prescribe them for patients over 65. Hospitals have cut their use by over 40% since 2018.Market data shows the shift: second-generation antihistamines now make up 78% of the $4.7 billion global market. First-generation sales are dropping 3.5% a year among older adults. By 2030, they may be under 10% of the market - and likely restricted to very short-term use.
New drugs are coming. In 2023, the FDA approved olopatadine nasal spray, which has zero anticholinergic activity. Researchers are now testing H4 receptor-selective antihistamines that may eliminate all off-target effects. The future of allergy treatment is precise - not broad.
Final Thought: Your Body Isn’t Broken - Your Medicine Might Be
If you’ve been living with dry mouth, constipation, or urinary problems for years and thought it was just “getting older,” think again. You might be mistaking a drug side effect for aging. The good news? You don’t have to live with it. Switching to a second-generation antihistamine can undo these problems - often within days.Don’t wait for a hospital visit to realize your allergy pill is doing more harm than good. Your bladder, your gut, and your brain will thank you.
Can antihistamines cause urinary retention?
Yes, especially first-generation antihistamines like diphenhydramine. They block acetylcholine receptors in the bladder, weakening muscle contractions and tightening the urethral sphincter. This can lead to urinary retention - a condition where you can’t fully empty your bladder. It’s especially dangerous for men with enlarged prostates. Studies show 31% of men with moderate prostate symptoms develop acute urinary retention within 48 hours of taking diphenhydramine. Second-generation antihistamines like cetirizine or fexofenadine rarely cause this issue.
Is dry mouth from antihistamines dangerous?
Dry mouth isn’t just uncomfortable - it’s a health risk. Saliva protects your teeth from decay and fights bacteria. When antihistamines reduce saliva by 60-70%, your risk of cavities, gum disease, and oral infections rises sharply. Chronic dry mouth can also make swallowing difficult and increase the chance of choking. People on long-term first-generation antihistamines often develop dental problems they didn’t have before. Switching to a second-generation antihistamine or using sugar-free xylitol gum can reverse this.
Do all antihistamines cause constipation?
No. Only first-generation antihistamines like diphenhydramine, chlorpheniramine, and promethazine cause significant constipation. They slow gut movement by blocking acetylcholine in the intestines. Second-generation antihistamines - cetirizine, loratadine, fexofenadine - have minimal to no effect on bowel function. Studies show constipation affects 15-20% of users of first-generation drugs but only 3-5% of those using second-generation ones.
Are second-generation antihistamines really better?
Yes, and the evidence is clear. They work just as well for allergies but don’t block acetylcholine receptors. This means no dry mouth, no constipation, no urinary issues, and no brain fog. They last 24 hours, so you take one pill a day. They’re safer for older adults, people with prostate problems, and anyone with digestive or bladder issues. Patient satisfaction rates are 68% for second-generation drugs versus 49% for first-generation, mostly because side effects are so much milder.
Can antihistamines cause dementia?
Long-term use of first-generation antihistamines like diphenhydramine is linked to a higher risk of dementia. A seven-year study found users had a 54% increased risk. Each extra year of use - especially beyond 90 doses per year - raised the risk by another 20%. Diphenhydramine has the highest possible anticholinergic cognitive burden score (3.0). The American Geriatrics Society and European guidelines now warn against using these drugs in older adults. Switching to second-generation antihistamines may reduce this risk.
What should I do if I’m taking Benadryl for sleep?
Stop using it regularly. While diphenhydramine makes you sleepy, it also causes dry mouth, constipation, urinary issues, and cognitive decline. It disrupts natural sleep architecture and doesn’t improve sleep quality. Safer alternatives include melatonin (for short-term use), cognitive behavioral therapy for insomnia (CBT-I), or non-anticholinergic sleep aids like doxylamine (in low doses, and only occasionally). Talk to your doctor - there are better ways to sleep without risking your brain or bladder.

Kyle Swatt
November 18, 2025 AT 21:32Man I used to pop Benadryl like candy before bed thought it was just helping me chill
Turns out my dry mouth and constipation weren't just aging
Switched to loratadine and my tongue stopped feeling like sandpaper in 3 days
My gut thanked me too
Why the hell do pharmacies still sell this junk like it's harmless
It's not a sleep aid it's a slow poison for your brain
They should put a skull and crossbones on the bottle
And don't even get me started on the urinary stuff
My uncle ended up catheterized after one night of 'just helping him sleep'
We're letting Big Pharma sell cognitive demolition kits like they're cough syrup
It's not just side effects it's systemic neglect
Older folks don't need more drugs they need better ones
Second-gen antihistamines aren't a luxury they're a basic right
And yet here we are still letting grandma choke on diphenhydramine like it's tea
Someone needs to burn the old formulary
saurabh lamba
November 18, 2025 AT 22:58so like... antihistamines = dementia? 😳
bruh i just want to sleep
also my cat is allergic to my breath
what do i do now?? 😭
Kiran Mandavkar
November 19, 2025 AT 10:34Of course you're surprised
You swallow pharmaceuticals like they're gummy vitamins
Do you even know what acetylcholine does?
No you don't
You just want your sneezes to stop and your brain to shut off
That's not medicine that's surrender
The body isn't broken your pharmacological ignorance is
Second-gen antihistamines have been available since the 90s
And yet here you are still poisoning your M3 receptors like a caveman with a pharmacy
It's not the drugs it's you
You don't read labels you don't research you just click buy
And now you're shocked your kidneys are tired
Wake up
The future of medicine is precision
Not shotgun blasts of anticholinergic garbage
And if you think this is just about allergies you're even dumber than I thought
Eric Healy
November 20, 2025 AT 04:46so i was on benadryl for like 10 years
then i started forgeting where i put my keys
and my wife said i was like a zombie
switched to zyrtec
now i remember my own name
also my poop is back to normal
who knew
also i found out my night time cold med had benadryl in it
so i threw out all my 'sleep aids'
turns out i was just drugged
not sleeping
and no i dont care if its otc
its still a drug
and it wrecked my brain
Shannon Hale
November 22, 2025 AT 02:12OH MY GOD I JUST REALIZED
I've been taking diphenhydramine since 2017
for my allergies
and my dry mouth
and my constipation
and my urinary issues
and my brain fog
and my fear of falling
and my dental decay
and my husband saying i'm not the same person
AND I THOUGHT IT WAS JUST AGING
IT WASN'T AGING
IT WAS A DRUG
I'M GOING TO THE PHARMACY RIGHT NOW
I'M GETTING LORATADINE
AND I'M THROWING OUT EVERY NIGHTTIME PILLS IN MY CABINET
MY BRAIN IS GOING TO BE FINE
MY BLADDER IS GOING TO BE FINE
MY TEETH ARE GOING TO BE FINE
AND I'M NEVER GOING BACK
Holli Yancey
November 22, 2025 AT 16:50I've been on cetirizine for years and I never realized how much better I felt until I read this
My mom was on Benadryl for sleep and she started having trouble walking
We didn't connect it until she got dizzy and fell
Switching her to loratadine was like turning on a light
She didn't even know she was foggy
It's scary how normal these side effects become
Like you just accept dry mouth as part of getting older
But it's not
It's a warning
And we're all just ignoring it
Thanks for putting this out there
I'm sharing it with my whole family
Jessica Healey
November 23, 2025 AT 05:47i just started taking zyrtec and my mouth is no longer a desert
i cried
really
i was so thirsty all the time
and now i can taste my coffee again
also my poop is back
like actual poop
not brick
and i can pee without feeling like i'm trying to open a stuck jar
why did no one tell me this was a thing
i thought i was just getting old
turns out i was just drugged
thank you
Levi Hobbs
November 23, 2025 AT 07:06I've been a nurse for 18 years, and I see this every single day.
Grandma takes Benadryl for allergies, then gets confused, then falls, then ends up in rehab.
It's not rare.
It's routine.
And we don't even question it.
Why? Because it's OTC.
Because it's cheap.
Because it's 'just a pill.'
But it's not.
It's a neurological wrecking ball.
And we're letting people walk into pharmacies and grab it like candy.
We need better education.
Pharmacists need to flag it.
Doctors need to ask.
Families need to speak up.
This isn't just medical advice.
It's a public health emergency.
henry mariono
November 24, 2025 AT 14:06My dad was on diphenhydramine for years.
He never complained.
He just got quieter.
Slower.
More forgetful.
I thought it was dementia.
Turns out it was the medicine.
We switched him to Allegra.
Within two weeks, he was asking about his old band again.
He remembered his wedding anniversary.
He laughed.
He didn't need to be 'fixed.'
He just needed a better pill.
Thank you for writing this.
I'm printing it out for his doctor.
kora ortiz
November 25, 2025 AT 01:27THIS CHANGED MY LIFE
Switched from Benadryl to Zyrtec
My dry mouth? Gone
My constipation? Gone
My brain fog? Gone
My sleep? Actually better
I didn't know I was sick
Now I feel like a new person
Don't wait for a hospital visit
Check your cabinet
Read the label
Change today
Your future self will hug you
Jeremy Hernandez
November 25, 2025 AT 07:24big pharma wants you to be old and confused
so they can sell you more pills
benadryl is a mind control drug disguised as allergy relief
they've been doing this since the 50s
they don't care if you get dementia
they care about your prescription refill rate
read the label
look for 'diphenhydramine'
if it's there
throw it out
and tell everyone you know
they're poisoning your grandma
and your dad
and your uncle
and you
don't be a sheep
Tarryne Rolle
November 26, 2025 AT 04:23It's funny how people act like this is some groundbreaking revelation
Anticholinergics have been known to cause cognitive decline since the 70s
It's not a surprise
It's a predictable consequence of lazy medicine
People want quick fixes
So they get slow destruction
And then they're shocked when their memory fades
It's not the body failing
It's the system failing
And you're all just blaming aging
When the real villain is the $0.99 bottle on the shelf
Stop being passive
Stop accepting
Start reading
Or stop pretending you care
Joseph Townsend
November 26, 2025 AT 09:09I took Benadryl for 15 years
Thought it was helping me sleep
Turns out I was just in a chemical fog
My wife said I'd become a ghost
Not emotionally
Physically
I'd stop talking mid-sentence
Forget where I put my glasses
Walk into walls
Switched to loratadine
Now I can remember my own birthday
And I don't need to pee every hour
And my mouth isn't a desert
It's like I woke up from a 15-year coma
And no one told me I was asleep
Bill Machi
November 26, 2025 AT 17:15Why are we letting corporations sell neurotoxins to seniors like they're cough drops?
This isn't freedom
This is negligence
They know the risks
They know the data
They still put it in every cold medicine
Because profit > people
And we're all complicit
We buy it
We take it
We don't ask questions
Until it's too late
And then we cry
While the same companies sell us dementia drugs
It's a cycle
And it's designed
Don't be a customer
Be a rebel
Read the label
Refuse the poison
Gordon Mcdonough
November 26, 2025 AT 17:51so i just checked my medicine cabinet
and i found 3 different things with diphenhydramine
nighttime cold med
allergy pill
and that 'sleep aid' i bought on sale
oh my god
i've been taking this for years
and i thought i was just tired
and dry
and constipated
and forgetful
turns out i was just poisoned
i'm throwing all of it out
and i'm telling everyone i know
and i'm gonna write a letter to the FDA
and i'm gonna make my mom switch too
and i'm gonna make my brother switch
and i'm gonna make my sister switch
and i'm gonna make my best friend switch
because no one should live like this
not anymore