Medication Interaction Checker
This tool identifies potential interactions between medications based on known medical data. It is not a substitute for professional medical advice. Always consult your doctor or pharmacist before making changes to your medication regimen.
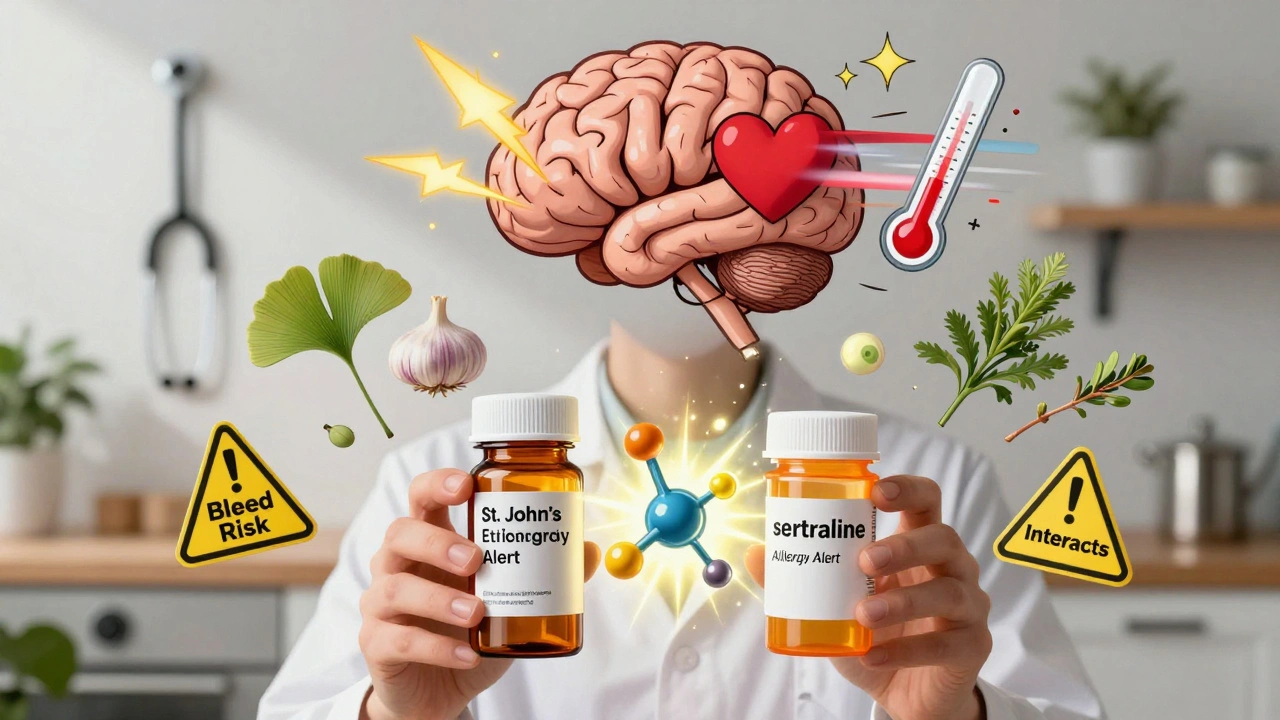
Not all medicines are created equal-even when they treat the same condition. Whether you're taking a prescription pill, an over-the-counter pain reliever, or a herbal supplement labeled "natural," each type of medication comes with its own set of risks. And those risks aren't always obvious. A skin rash from an antibiotic might be easy to spot, but a dangerous interaction between St. John’s Wort and your antidepressant? That could sneak up on you without warning.
Prescription Drugs: Same Active Ingredient, Different Risks
Generic versions of brand-name drugs are supposed to work the same way. The FDA requires them to contain the same active ingredient, in the same strength, and to be absorbed into your body at nearly the same rate. In fact, studies show that for most drugs-especially heart medications like beta-blockers, statins, and blood pressure pills-generics perform just as well as the originals.
But here’s the catch: the inactive ingredients are different. Things like lactose, corn starch, dyes, or preservatives. If you’re lactose intolerant, a generic version of your thyroid medication might give you bloating and diarrhea-not because the drug isn’t working, but because of the filler. Same goes for people allergic to sulfites or soya lecithin. These aren’t listed prominently on the bottle, so unless you check the full ingredient list, you won’t know.
And then there are the narrow therapeutic index (NTI) drugs. These are the ones where even a tiny change in blood level can cause big problems. Think levothyroxine for hypothyroidism, or warfarin for blood thinning. Switching from one brand to another, or even between two different generic makers, can throw your levels off. One study found patients on generic antiepileptic drugs had more seizures and needed more doctor visits after switching. That’s not theory-it’s real, documented risk.
Over-the-Counter (OTC) Medications: Just Because It’s Available Doesn’t Mean It’s Safe
Aspirin, ibuprofen, acetaminophen-these are the workhorses of the medicine cabinet. But they’re not harmless. Long-term use of NSAIDs like ibuprofen can damage your stomach lining or kidneys. Acetaminophen, when taken in high doses or mixed with alcohol, can cause liver failure. And many people don’t realize they’re doubling up: a cold medicine might already contain acetaminophen, and if you take a separate painkiller on top, you’re overdoing it.
OTC drugs are regulated, but that doesn’t mean they’re risk-free. The labels are full of warnings, but most people skip them. And if you’re taking other prescriptions, interactions are common. For example, mixing ibuprofen with blood pressure meds can make them less effective. Antihistamines in sleep aids can cause confusion in older adults. These aren’t rare events-they happen every day.
Herbal Supplements and Complementary Medicines: The Wild West of Medicine
This is where things get dangerous. Unlike prescription and OTC drugs, herbal supplements don’t need FDA approval before hitting the shelf. Companies don’t have to prove they work. They don’t have to list all ingredients accurately. And they rarely test for interactions with other medications.
Echinacea? It can trigger asthma attacks or severe allergic reactions in some people. Feverfew? It may cause uterine contractions-dangerous during pregnancy. Ginkgo, garlic, and ginger? All of them can thin your blood. If you’re on warfarin, that’s a recipe for internal bleeding.
St. John’s Wort is one of the most common culprits. People take it for mild depression, not realizing it can cause serotonin syndrome when mixed with SSRIs like sertraline or fluoxetine. Symptoms? Tremors, high fever, rapid heartbeat, low blood pressure. It’s not a mild side effect-it’s a medical emergency.
And don’t assume "natural" means safe. A 2023 review found that nearly 1 in 5 people using herbal supplements didn’t tell their doctor. That’s a problem because doctors can’t help if they don’t know what you’re taking.

Why Switching Between Brands and Generics Can Backfire
Many people switch to generics to save money. And for most drugs, it’s fine. But for NTI drugs, consistency matters. Switching between different generic versions of levothyroxine, for example, can cause your TSH levels to swing. One manufacturer’s version might absorb slightly faster than another. That’s not a flaw-it’s normal variation. But for someone relying on precise hormone levels, even a 5% difference can mean fatigue, weight gain, or heart palpitations.
Some patients report feeling worse after switching-even when lab tests say everything’s normal. That’s because side effects aren’t always measurable in blood work. You might feel jittery, nauseous, or mentally foggy. Those are real symptoms, even if the drug is "bioequivalent."
Doctors often don’t warn patients about this. Insurance companies push generics, and pharmacists automatically substitute unless you say otherwise. But if you’re on warfarin, thyroid meds, or seizure drugs, ask your pharmacist: "Is this the same manufacturer as before?" If they say no, talk to your doctor before taking it.
What You Can Do to Stay Safe
- Know your ingredients. Check the label. If you’re allergic to lactose, soy, or dyes, look for versions that list "lactose-free" or "dye-free."
- Keep a list. Write down everything you take-even ginseng or turmeric capsules. Bring it to every appointment.
- Don’t assume "natural" is safe. Herbal supplements can be just as powerful-and just as dangerous-as prescription drugs.
- Ask before you switch. If you’re on a narrow therapeutic index drug, don’t let your pharmacist substitute without checking with your doctor first.
- Watch for new symptoms. If you start feeling different after a new prescription or supplement, don’t brush it off. Track when it started and what you changed.
- Limit alcohol. It interacts with antibiotics, painkillers, antidepressants, and even some supplements. Even one drink can cause dizziness, nausea, or liver stress.
When to Call Your Doctor
Not every side effect needs an emergency room visit-but some do. Call your doctor if you notice:
- A sudden rash, swelling, or trouble breathing (signs of an allergic reaction)
- Unexplained bruising or bleeding (possible blood thinner interaction)
- Severe dizziness, confusion, or rapid heartbeat (could be serotonin syndrome)
- Worsening of your condition after switching medications
- Any new symptom that started within 48 hours of starting a new drug or supplement
Side effects aren’t always obvious. Sometimes they’re mistaken for the illness itself. A headache from a new blood pressure pill? Maybe you think it’s stress. A stomach ache from a generic antibiotic? Maybe you blame your diet. But if it’s new, it’s worth investigating.
Are generic drugs always as safe as brand-name ones?
For most medications, yes. Generic drugs must meet the same standards for active ingredients and effectiveness as brand-name versions. But for narrow therapeutic index drugs like warfarin or levothyroxine, even small differences in how the body absorbs the drug can matter. In those cases, sticking with the same manufacturer helps avoid side effects. Also, inactive ingredients can trigger allergies or intolerances-so check the label.
Can herbal supplements really interact with prescription drugs?
Absolutely. St. John’s Wort can cause serotonin syndrome when taken with antidepressants. Ginkgo, garlic, and ginger can increase bleeding risk with blood thinners like warfarin. Echinacea can interfere with liver-metabolized drugs, making them less effective or more toxic. Many people don’t realize they’re taking supplements, and doctors often don’t ask. Always tell your provider what you’re using-even if you think it’s "just a tea."
Why do some people feel worse after switching to a generic?
It’s not always the active ingredient. Differences in fillers, coatings, or how quickly the pill dissolves can affect how your body responds. For people with sensitivities, a new filler can cause stomach upset or allergic reactions. For those on narrow therapeutic index drugs, even minor absorption changes can lead to symptoms like fatigue, mood swings, or seizures. It’s not placebo-it’s real physiological variation.
How do I know if my medication has a narrow therapeutic index?
Common examples include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin and carbamazepine (for seizures), and lithium (for bipolar disorder). Your pharmacist or doctor can tell you if your drug falls into this category. If it does, avoid switching between different generic brands without medical supervision. Consistency in the manufacturer matters.
Is it safe to take supplements with my prescription meds?
Not without checking. Supplements aren’t tested for interactions like prescription drugs are. Even something as simple as vitamin K can make warfarin less effective. Calcium supplements can interfere with thyroid medication if taken at the same time. Always ask your pharmacist: "Does this supplement interact with any of my prescriptions?" If they don’t know, ask your doctor. Better safe than sorry.
Final Thought: Your Body Is Your Best Alarm System
You know your body better than any drug label. If something feels off after starting a new medicine-whether it’s a pill from the pharmacy or a bottle of herbal drops-don’t ignore it. Side effects aren’t always listed. They aren’t always predictable. But they’re always real. The goal isn’t to avoid all medication. It’s to use it wisely. Know what you’re taking. Ask questions. Track changes. And never assume "natural" means harmless.

Angela R. Cartes
December 9, 2025 AT 20:36Lisa Whitesel
December 10, 2025 AT 20:52Larry Lieberman
December 12, 2025 AT 08:32Courtney Black
December 12, 2025 AT 23:42iswarya bala
December 14, 2025 AT 19:42Anna Roh
December 16, 2025 AT 07:12om guru
December 16, 2025 AT 22:11Richard Eite
December 18, 2025 AT 12:41Katherine Chan
December 20, 2025 AT 03:42