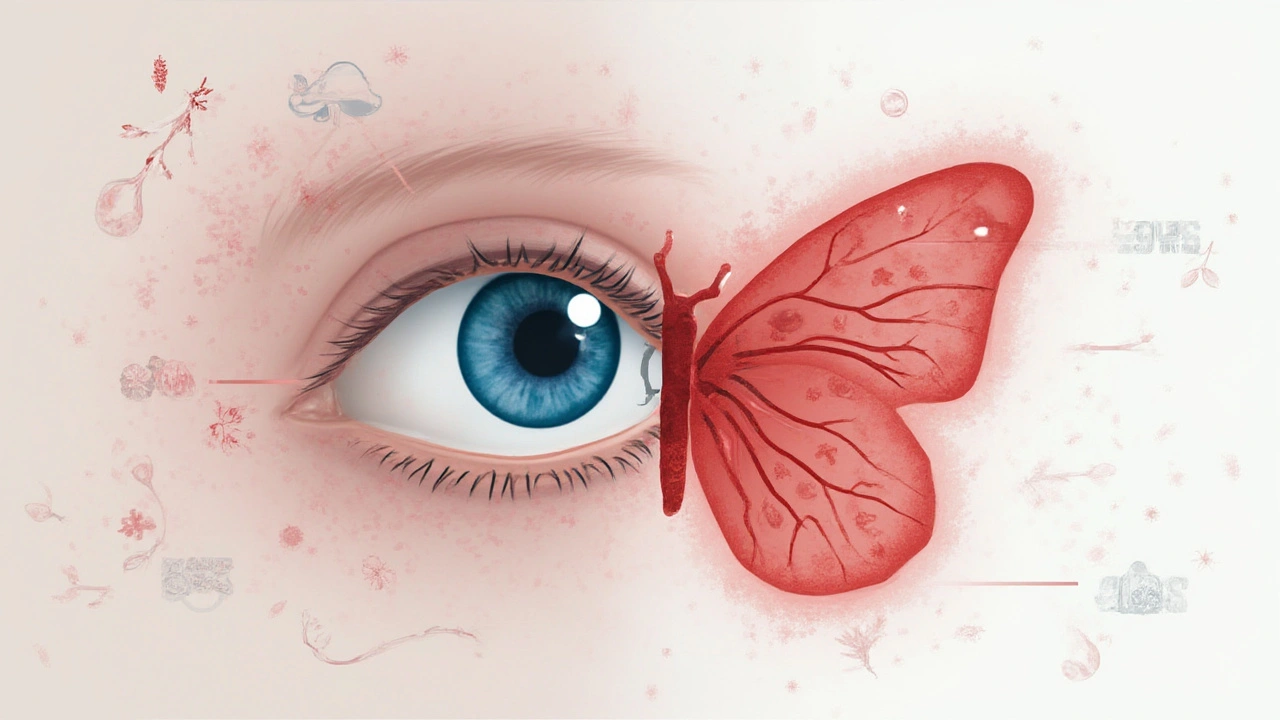
Barely slept? Maybe your eyes look red, but did you know a persistent red eye could mean something bigger than you think? Forget the usual suspects like allergies or staring at screens for too long—for some, eye redness is actually a blinking red flag that something’s up with their thyroid. It’s not just the stuff of rare textbooks. It happens to regular people like you and me. The trick is, not many connect the dots between the glands in your neck and the whites of your eyes. You’d be forgiven for missing the connection. I know it sounds a bit sci-fi, but the link is quite real and worth understanding, especially if you or someone you care about is struggling with unexplained red, puffy, or irritated eyes. Let’s clear things up and see what’s behind it all.
Understanding the Connection: How Thyroid Disease Affects the Eyes
First, let’s lay out how the thyroid and your eyes even cross paths. The thyroid gland lives low in your neck and controls a lot, from your energy levels to how you gain or lose weight. When things go off balance—hyperthyroidism if it goes into overdrive, hypothyroidism if it slows down—the rest of you starts noticing, including your eyes. One of the most notorious matches here is something called Thyroid Eye Disease (sometimes called TED or Graves’ ophthalmopathy), which happens mostly in people with Graves’ disease, a type of overactive thyroid. The immune system, in a bizarre mix-up, starts attacking tissues around the eyes, thinking they’re the enemy.
As these tissues get inflamed, you see redness. But it’s not always bright scarlet redness—sometimes it’s more like a persistent bloodshot look that eye drops won’t fix. Swelling, bulging eyes (medical folks call this exophthalmos), and discomfort often show up too. And it’s not just the look—it’s the feel. People describe a constant itch, dryness, watery eyes, light sensitivity, or the sensation that there’s sand gritty in their eyes. I’ve heard stories from folks in Bristol chatting in coffee shops: their eyes looked wild, almost startled, and it turned out to be their thyroid giving them a hard time.
Women are more affected than men, especially those between 30 and 50, but you’ll spot it in blokes as well. Another twist? Smoking ups your odds of eye problems with thyroid disease—double, in fact. There was a study at Moorfields Eye Hospital in London where researchers noticed that smokers with Graves’ disease were far more likely to develop the eye complications than non-smokers. Not a scare tactic—just real talk. Redness isn’t always dramatic either. It can creep up, making you think you’re just tired, allergic, or got poked in the eye when in reality, your immune system is starting a row with your eye tissues. The British Thyroid Foundation put it simply: If red, puffy eyes linger, get checked for thyroid disease, especially with other symptoms like weight swings or feeling jittery.
Spotting Symptoms and Signs: What to Watch For Beyond Redness
The thing is, lots of folks brush off eye redness as no big deal, using every over-the-counter drop and allergy remedy under the sun. But when it keeps coming back—or comes bundled with other weird signs—it’s a hint to look deeper. Yes, you might get the dramatic look of bulging eyes, but honestly, the symptoms can be much sneakier than that.
Redness can hide amongst swelling, watering, mild pain, or a scratchy feeling. You might blame work, kids, sleepless nights, or Manchester weather, but there’s a pattern when the thyroid’s involved. The area around the eye feels tight or puffy; blinking is uncomfortable, and some even struggle to close their eyes all the way. Headaches and double vision can sneak in. Patients sometimes describe a stabbing pain behind their eye or soreness just moving them around. In some noticeable cases, people look almost permanently surprised, with the whites of their eyes visible above and below the colored part. That’s a dead giveaway that the eye muscles and tissues are inflamed and pushing things forward.
Here’s an everyday example: Mary, a yoga instructor from Bath, thought her trouble focusing and constant red eyes were just part of getting older. She ignored it until one morning, mascara stung like crazy and her boyfriend noticed her eyes looked "weird and puffy." A blood test showed overactive thyroid hormones and, just to confirm, an ophthalmologist diagnosed thyroid-related eye disease. The tipping point? Her eye redness hadn’t gone away for weeks, and she noticed her vision sometimes blurred in one eye when she glanced sideways.
This brings me to some key red flags to look out for:
- Redness that won’t quit, no matter how much you rest or treat allergies
- Constant feeling of dry or gritty eyes
- Excessive watering, especially outdoors
- Puffiness, especially above and below the eyes
- Pain or aching behind the eyes
- Sudden double vision or trouble seeing straight
- Difficulty moving your eyes side to side
- A wide-eyed or surprised appearance
If you have any of these—especially with weight changes, anxiety, feeling too hot or cold, or a sudden burst of energy (or exhaustion)—mention it to your GP. Don’t wait. Catching thyroid problems early can make a huge difference in how your eyes recover.
Treating and Managing Eye Redness from Thyroid Disease
Let’s get to the part that really matters: what can you do about it? There isn’t one magic bullet, but the good news is, with help, most people manage symptoms and protect their eyes. It nearly always starts with controlling the thyroid itself. If the thyroid’s running wild, no amount of eye drops will really solve the root of the problem. Your NHS endocrinologist will probably tweak your thyroid medication—sometimes you’ll need radioiodine, other times tablets or even surgery, depending on how wild things are.
For the eyes, you might get a referral to an oculoplastic surgeon or ophthalmologist who knows about thyroid eye disease. Classic advice: stop smoking, completely. Even cutting down won’t do. Smoking links so tightly to bad eye outcomes in thyroid disease, it’s almost not fair. Another big tip—wear sunglasses outside, even in Bristol’s ever-cloudy weather. They block both sun and wind, keeping eyes from getting drier. Use artificial tears during the day and thicker lubricating gels at bedtime. This isn’t glamorous, but it works, and it’s safe. Some people use a humidifier near their desk or bed to keep air moist, especially in winter or with central heating, as dryness makes irritation worse.
Avoid rubbing your eyes, even if they itch—it only makes inflammation worse. If swelling gets bad, you might get prescribed steroid pills or drops for a while. In severe cases, there are targeted medicines now, like teprotumumab, approved in the US and being evaluated in the UK, which specifically treat the underlying inflammation in the tissues behind the eyes. And if your eyelids won’t close at night, special tape or eye shields can prevent the cornea from drying out and getting scratched. For people with extreme bulging or double vision, surgery is sometimes needed—to move eye muscles, reshape eyelids, or create space behind the eye. It sounds scary but has made a world of difference for many, getting eyes back to normal and stopping the cycle of redness, pain, and fear of looking "unwell" or "different."
Keep your GP updated about any vision changes or pain. It’s not vain or silly to push for a specialist appointment if it feels like more than "just red eyes." In Bristol, and pretty much everywhere in the UK, these referrals are taken seriously, especially if you have thyroid imbalance in your medical history. Do what you can to avoid triggers: give your eyes a tech break (that endless scroll makes irritation worse), get enough sleep, and eat a balanced diet rich in vitamin A and omega-3s. It’s simple, but every bit helps. Some eye creams and over-the-counter drops can do more harm than good, so stick with what your eye doctor recommends.
If you have a family history of thyroid disease, or anyone in your family has struggled with eye redness that didn’t go away, be upfront with your GP. And keep an honest eye on yourself if you’re managing thyroid issues already. Quick action makes all the difference. Your eyes aren’t just windows to your soul—sometimes they’re the early warning system that something deeper needs your attention.

Chelsey Gonzales
July 24, 2025 AT 16:13i had no idea red eyes could be tied to your thyroid 😳 i thought it was just from too much coffee and scrolling at 2am. my aunt had this weird bulgy eye thing and everyone thought she was mad, turns out it was graves disease. she quit smoking and started on meds and her eyes went back to normal. mind blown.
Kelly Library Nook
July 24, 2025 AT 20:29The assertion that thyroid eye disease is underdiagnosed is statistically unsupported. Peer-reviewed data from the Journal of Clinical Endocrinology & Metabolism (2022) indicates a diagnostic accuracy rate of 87% among endocrinology-referral populations in the U.S. The anecdotal framing of this article is misleading and risks inducing unnecessary medical anxiety among otherwise healthy individuals presenting with benign conjunctival hyperemia.
Crystal Markowski
July 26, 2025 AT 00:21Thank you for writing this with such care. So many people dismiss eye discomfort as "just tired" or "allergies," and it’s heartbreaking when it’s something deeper. I’ve seen friends go years without answers because doctors didn’t connect the dots. If you’re noticing persistent redness, puffiness, or vision changes-especially with fatigue, weight shifts, or anxiety-please don’t wait. Advocate for yourself. Thyroid eye disease is treatable, but early detection saves vision and peace of mind. You’re not being dramatic. You’re being smart.
Charity Peters
July 27, 2025 AT 15:45my eyes have been red for months. i thought it was dry air. maybe i should get my thyroid checked.
Faye Woesthuis
July 29, 2025 AT 13:07Stop being lazy. If your eyes are red, see a doctor. Don’t wait for some blog to tell you it’s your thyroid. You’re just scared to face the truth: you’re sleep-deprived, dehydrated, and probably addicted to your phone.
raja gopal
July 30, 2025 AT 05:15I’m from India, and here, many people think eye redness is just from heat or stress. But I’ve seen my cousin suffer with bulging eyes and double vision-she was misdiagnosed for a year. When they finally checked her thyroid, everything made sense. Please, if you’re reading this and have similar symptoms, don’t ignore it. It’s not vanity. It’s your health. And yes, quitting smoking helps-my cousin quit and her eyes improved in 4 months.
Samantha Stonebraker
July 31, 2025 AT 11:30There’s something quietly powerful about the body whispering before it screams. Red eyes aren’t just a cosmetic nuisance-they’re a language. A language of inflammation, of immune betrayal, of systems out of sync. And yet, we’ve been trained to numb them with drops and ignore them with caffeine. Maybe the real medicine isn’t just in the pills or the scans, but in learning to listen-to the grit in your gaze, the ache behind your sockets, the way your reflection looks back at you and says, "Hey. Something’s off. Pay attention."
Kevin Mustelier
August 2, 2025 AT 06:40Wow. Just... wow. 😮 I’ve been reading this like a novel. Who knew thyroid disease could turn your eyes into a horror movie? And smoking? Come on. You’re basically lighting a match to your eyeballs. 🚬🔥 I’m getting my bloodwork done tomorrow. Also, I’m gonna start wearing sunglasses indoors now. Just in case.