Daily Task Functionality Assessment
Assess Your Daily Functionality
This tool helps you evaluate your ability to perform everyday tasks. Occupational therapy focuses on enabling you to perform activities that matter most to you. Your results will help you understand where occupational therapy might provide the most value.
Get dressed
Prepare a simple meal
Take a shower
Get out of bed
Write or type for 10 minutes
Drive a car
Your Functional Assessment Results
Functional Score:
Score Range: 0-30
What occupational therapy can help:
Based on your scores, occupational therapists can help you improve your daily function through:
- Adaptive equipment for tasks you find challenging
- Energy conservation strategies to reduce fatigue
- Task-specific practice for improved endurance
- Environmental modifications for safer task performance
When it comes to keeping muscles functional, many people think of doctors, surgeons, or gyms. Occupational Therapy is a health‑care profession that focuses on enabling people to perform everyday tasks despite physical or cognitive challenges. It becomes especially powerful when paired with a clear understanding of Skeletal Muscle Conditions are disorders that affect the structure or performance of the muscles attached to the skeleton, ranging from inherited myopathies to injury‑induced weakness. This article walks you through why OT matters, what therapists actually do, and how you can make the most of it.
Key Takeaways
- Occupational therapy targets functional goals-getting you back to the tasks that matter most.
- Therapists assess muscle strength, range of motion, and daily‑life barriers before building a plan.
- Interventions blend exercise, adaptive equipment, and habit‑retraining to protect joints and boost endurance.
- Collaboration with physical therapy and medical teams improves outcomes for conditions like myopathy, muscular dystrophy, and post‑surgical weakness.
- Evidence shows patients who engage in OT see a 30‑40% improvement in independence scores within six months.
Understanding Skeletal Muscle Conditions
Muscle problems can be grouped into three broad categories:
- Neuromuscular disorders - diseases that affect nerve‑muscle communication, such as amyotrophic lateral sclerosis (ALS) or spinal muscular atrophy.
- Myopathies - intrinsic muscle diseases like Duchenne muscular dystrophy or limb‑girdle muscular dystrophy.
- Acquired injuries - strains, tears, or post‑operative weakness that limit force generation.
Regardless of the cause, the core effect is reduced ability to generate force, maintain joint stability, and perform activities of daily living (ADLs). Without intervention, secondary issues such as joint contracture, pain, and loss of independence quickly follow.
What Occupational Therapy Is (and Isn’t)
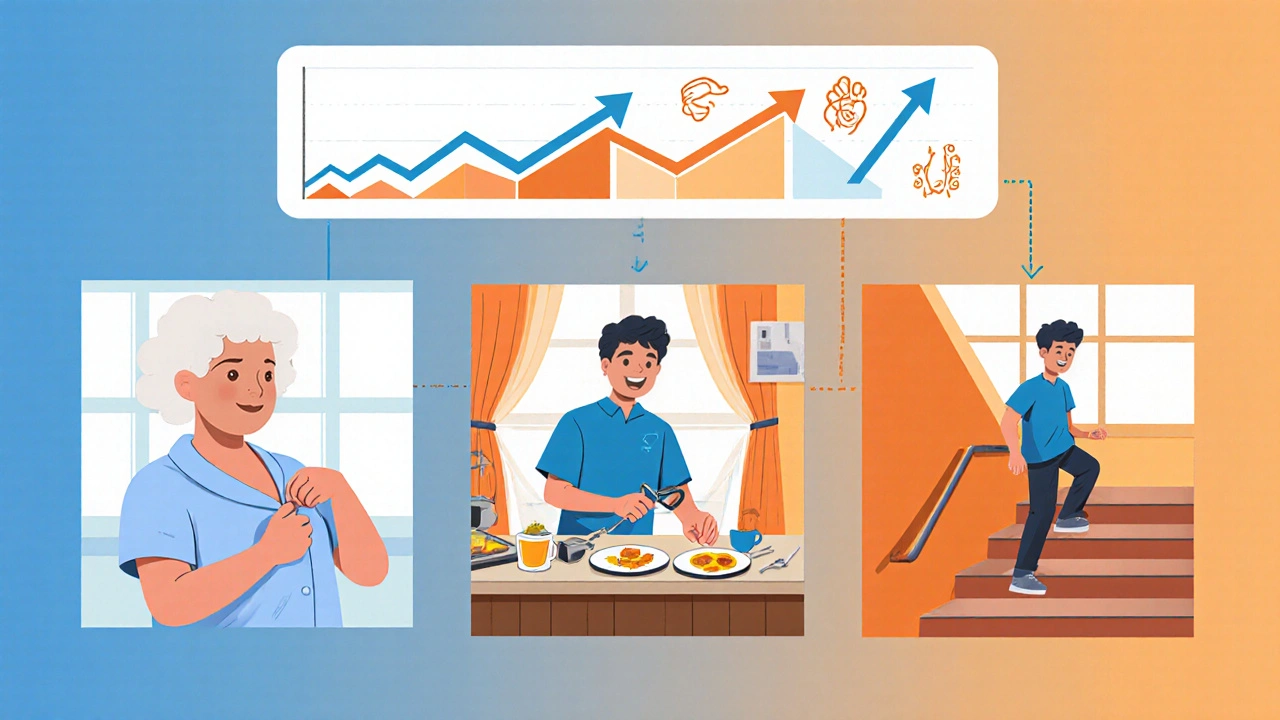
Physical Therapy focuses on restoring movement, strength, and balance through exercise and manual techniques. In contrast, occupational therapy looks beyond pure movement. It asks: “Can this person get dressed, cook a meal, or use a computer without pain or fatigue?” The answer drives every assessment and treatment decision.
OT is patient‑centered, meaning the therapist tailors goals to the individual’s lifestyle, home environment, and personal priorities. A teenager with a muscular dystrophy may want to play video games, while an older adult recovering from a hip fracture cares about getting out of the bathtub safely. Both situations call for different strategies, even if the underlying muscle weakness looks similar.

How OT Addresses Muscle Conditions
Therapists follow a systematic process that can be broken down into four stages:
- Comprehensive assessment - measuring strength, range of motion, and endurance; observing how the person performs key ADLs; and identifying environmental barriers.
- Goal setting - translating assessment findings into functional objectives, such as “button a shirt within 30 seconds” or “prepare a simple breakfast without pain.”
- Intervention planning - selecting a blend of exercises, adaptive equipment, and habit‑retraining techniques.
- Progress monitoring - using standardized tools like the Canadian Occupational Performance Measure (COPM) to track gains and adjust the plan.
OT Techniques and Tools for Muscle Health
Below are the most common levers therapists pull:
- Muscle strength training - low‑load, high‑repetition exercises that improve endurance without overloading fragile fibers. Therapists often incorporate functional tasks (e.g., lifting a grocery bag) to keep training relevant.
- Range‑of‑Motion (ROM) activities - gentle stretching or joint mobilization to prevent contracture. Maintaining full ROM is a cornerstone of long‑term independence.
- Assistive technology - devices such as adaptive utensils, voice‑activated smart home controls, or lightweight exoskeletons that offset weakness.
- Task‑specific practice - repeating the exact activity a person wants to master, like buttoning a shirt or typing on a keyboard. Repetition reinforces neural pathways and builds confidence.
- Energy‑conservation strategies - teaching pacing, sequencing, and the use of “rest breaks” to avoid fatigue during daily chores.
Assistive Technology includes both low‑tech tools (grab bars, elastic shoelaces) and high‑tech solutions (tablet‑based apps for voice control). Proper selection can reduce the force required for everyday tasks by up to 50%, giving muscles a chance to recover.
Collaboration With Physical Therapy and Other Professionals
OT rarely works in isolation. A coordinated care team usually looks like this:
| Aspect | Occupational Therapy | Physical Therapy |
|---|---|---|
| Primary Goal | Functional independence in daily tasks | Improved movement mechanics and strength |
| Typical Interventions | Adaptive equipment, task‑specific practice, energy‑conservation training | Therapeutic exercises, gait training, manual therapy |
| Outcome Measures | COPM, ADL performance scores | Timed Up‑and‑Go, 6‑Minute Walk Test |
| Patient Population Emphasis | Adults seeking independence, children with developmental challenges | Athletes, post‑surgical patients |
When OT and PT share assessment data, they can align strength exercises with real‑world tasks, creating a seamless bridge from clinic to kitchen counter.
Measuring Success: Evidence‑Based Practice
Research from the Journal of Hand Therapy (2023) shows that participants receiving combined OT/PT interventions improved their ADL scores by an average of 35% versus a 15% gain in PT‑only groups. Another systematic review (2024) highlighted that early OT involvement-within the first two weeks of a muscle injury-reduced long‑term contracture risk by 22%.
Therapists rely on quantitative tools (dynamometry for grip strength) and qualitative feedback (patient‑reported pain). The blend ensures that progress isn’t just numbers on a chart but real‑world improvements like “I can now climb the stairs without holding the rail.”
Practical Tips for Patients, Caregivers, and Clinicians
- Ask your therapist to demonstrate each adaptive tool before you leave the clinic; hands‑on practice beats watching a video later.
- Keep a simple log of daily activities and fatigue levels. Patterns in the log help the OT fine‑tune intensity.
- Integrate strength exercises into real tasks-lift a weighted basket while cooking, or practice buttoning while seated.
- Don’t wait for pain to become severe before seeking OT; early intervention preserves joint range and muscle length.
- Coordinate with the medical team about medication side‑effects that may affect muscle tone, such as steroids, so the OT can adjust the plan.
Frequently Asked Questions
When should I consider occupational therapy for a muscle condition?
If you notice difficulty with everyday tasks-dressing, cooking, writing-or if a doctor mentions a risk of contracture, booking an OT assessment within the first month is ideal.
Is occupational therapy covered by the NHS?
Most NHS trusts provide OT services for chronic or acute muscle conditions when referred by a GP or specialist. Private clinics also offer faster access if you prefer.
What’s the difference between OT and a personal trainer?
A personal trainer designs fitness programs for healthy bodies, while an occupational therapist creates functional solutions for people whose muscles limit daily life. OT integrates medical knowledge, adaptive equipment, and environmental modifications.
Can OT help after a muscle surgery?
Yes. Post‑operative OT focuses on pain‑free movement, scar management, and returning to tasks like driving or writing as soon as medically safe.
How long does an OT program usually last?
Programs are highly individual. Some people see measurable gains in 6‑8 weeks, while chronic conditions may require ongoing sessions for months or years.
Occupational therapy isn’t a one‑size‑fits‑all prescription; it’s a flexible, client‑driven approach that transforms muscle weakness into real‑world capability. Whether you’re dealing with a genetic myopathy, a sports injury, or age‑related muscle loss, a qualified OT can help you reclaim independence, reduce pain, and stay active in the activities you love.

Ritik Chaurasia
October 22, 2025 AT 15:06Occupational therapy isn’t just a buzzword in Indian hospitals – it’s the bridge that lets people with muscle disorders actually live their lives.
From Delhi to small towns, therapists are already integrating adaptive gadgets that cut down on joint strain.
If you’re battling a myopathy, ask for a home‑assessment; the OT can redesign your kitchen layout in minutes.
Don’t wait for a crippled future – get the OT involved now.
Gary Marks
October 26, 2025 AT 20:39Reading this article feels like watching a toddler try to juggle flaming torches while we’re expected to applaud the effort.
First off, OT is not some magical wand that instantly reverses years of muscle degeneration – it’s hard work, patience, and a grind that most people aren’t willing to endure.
The author glosses over the brutal reality that many patients can’t even afford the pricey adaptive equipment, let alone the endless therapist visits that bleed your wallet dry.
Sure, a “30‑40% improvement” sounds shiny, but that statistic hides the fact that those gains are measured under controlled clinic conditions, not in the chaotic mess of real life where family members are exhausted and insurance companies love to say “not covered.”
Let’s not forget the hidden emotional toll – sitting through repetitive exercises day after day while feeling like a lab rat can drain the soul.
And the whole “energy‑conservation” spiel? It’s basically telling patients to move slower and accept their limitations, which is a covert way of keeping them docile.
The article pretends OT is a partnership, but in reality it’s a hierarchy where the therapist dictates what you can and cannot do, often without truly listening to your personal goals.
When the author mentions “task‑specific practice,” they fail to acknowledge that many daily tasks are impossible without major home renovations that most people can’t afford.
Adaptive utensils? Great, if you have the luxury of buying a new set of fancy gadgets every few months.
In my experience, the OT’s recommendations become another layer of bureaucracy that patients must navigate, adding stress instead of relief.
The collaboration with physical therapy sounds ideal, yet coordination between the two disciplines is notoriously fragmented, leaving patients with conflicting advice.
I’m also sick of the vague “early OT involvement” cue – who decides what “early” means? Your doctor, your insurance, or the therapist’s schedule?
Bottom line: OT can be useful, but it’s not the panacea the article tries to sell, and anyone reading this should approach it with a healthy dose of skepticism and a solid budget plan.
Steven Young
October 31, 2025 AT 03:12OT looks great on paper but the hidden agenda is obvious it serves the pharma‑industrial complex by keeping patients dependent on endless appointments it’s a subtle form of control saying the more you trust the system the safer you are
Holly Green
November 4, 2025 AT 09:45OT truly shines when therapists tailor activities to what matters most to the patient.
It’s not about fancy equipment, it’s about regaining independence.
Craig E
November 8, 2025 AT 16:17There’s a certain poetry to watching a therapist transform a mundane kitchen into a stage for empowerment.
When we consider the philosophical underpinnings, OT invites us to question what “function” really means – is it merely the ability to lift a cup, or the freedom to engage in a cherished ritual?
The color‑rich language of adaptive tools mirrors the vibrant possibilities they unlock.
Respectfully, I’d add that the therapist’s role is less of a director and more of a catalyst, gently nudging the client toward self‑discovery while honoring personal boundaries.
Eileen Peck
November 12, 2025 AT 22:50i think the best tip is to start with low‑tech solutions like elastic shoelaces or a simple grab bar-don’t overcomplicate things.
also keep a small journal of what feels easy and what s trigers fatigue it helps the ot fine‑tune the program.
typo note: its ok make mistakes, the therapist will catch them.
Sireesh Kumar
November 17, 2025 AT 05:23Listen, the drama of a teen with DMD suddenly being able to press a gaming controller is a saga worthy of a blockbuster!
Yet the everyday heroics-like a simple button‑up shirt-are what truly deserve applause.
Remember, every adaptive hack is a plot twist in the story of reclaiming life.
The OT is the unsung writer, penning endings where the protagonist triumphs.
Jonathan Harmeling
November 21, 2025 AT 11:56It is our moral duty to ensure that every individual who struggles with muscle weakness receives the most compassionate and evidence‑based care possible.
Occupational therapy, when applied ethically, reflects society’s commitment to dignity and independence.
Taylor Haven
November 25, 2025 AT 18:28There’s a subtle agenda woven into the narrative of occupational therapy that most people overlook.
The industry quietly promotes a culture of dependence, ensuring that patients keep coming back for assessments, device upgrades, and endless paperwork.
Meanwhile, insurance firms profit from the ad‑hoc nature of “custom” interventions, a perfect storm for profiteering.
Those “early interventions” are often just a ploy to lock patients into a long‑term billing cycle before they even realize the real costs.
Don’t be fooled by the glossy case studies; they rarely disclose the hidden fees that drain personal savings.
In truth, the most effective interventions are simple lifestyle adjustments that don’t require a therapist’s prescription.
Think critically about who truly benefits-often it’s not the patient, but the corporate entities behind the devices.
Stay vigilant, demand transparency, and question every recommendation that feels more like a sales pitch than a therapeutic necessity.
Vandermolen Willis
November 30, 2025 AT 01:01Hey everyone, great discussion! 😊
Just wanted to add that staying hydrated and taking micro‑breaks during tasks can really boost endurance.
Also, many apps now let you set reminders for those rest intervals-super handy! 👍
Mary Keenan
December 4, 2025 AT 07:34OT is overrated.
Kelly Brammer
December 8, 2025 AT 14:06While the benefits of occupational therapy are evident, it is essential to maintain rigorous standards and avoid over‑promising outcomes.
Clinicians must uphold ethical practices to ensure genuine patient progress.